Attending on the inpatient Infectious Disease service always stimulates discussion regarding management of bloodstream infections: What is the optimal duration? Can we use oral antibiotics? Do we need to document clearance of blood cultures? When these discussions lead to review of literature, one will find that the data is evolving in an attempt to answer these questions. Last month’s ID journal club included spirited discussions about one of these questions, led by our ID Division Chief, Dr. Mark Rupp.
Dr. Rupp reviewed an article by Canzoneri CN, et al: Follow-up blood cultures in gram-negative bacteremia: are they needed? Clinical Infectious Diseases. 2017;65(11):1776-9.
It is well accepted that patients with Staphylococcus aureus bloodstream infection (BSI) require follow-up blood cultures at day 2-4 to establish whether the infection should be classified as complicated, thus requiring at least 4 weeks of antibiotics. Unfortunately, many clinicians extrapolate from experience with S. aureus BSI and apply the same practice to patients with BSI due to gram-negative bacilli. There is little data to support routine follow-up blood cultures in patients with gram-negative bacilli BSI. Therefore, Canzoneri and colleagues at the University of Texas Health Science Center in Houston reviewed their experience in 500 patients with bloodstream infection during the year 2015.
 Of 500 patients with bloodstream infection, 383 (77%) had follow-up blood cultures. Of the 383 patients with follow-up blood cultures, 140 had a bloodstream infection due to gram-negative bacilli and only 8 (5.7%) follow-up blood cultures were positive. In contrast, 43 patients (20.8%) of patients with gram-positive cocci BSI had positive follow-up blood cultures. The only factor that predicted a positive follow-up blood culture in patients experiencing bloodstream infection due to gram-negative bacilli was fever at the time of the follow-up blood cultures. Other risk factors examined included whether the patient was receiving antibiotics, the presence of a central venous catheter or urinary catheter, neutropenia, HIV, diabetes, end-stage renal disease on hemodialysis, cirrhosis, ICU care, and mortality. Thus, 17 follow-up blood cultures had to be obtained in patients with gram-negative bacilli BSI in order to define one person with persistent bacteremia.
Of 500 patients with bloodstream infection, 383 (77%) had follow-up blood cultures. Of the 383 patients with follow-up blood cultures, 140 had a bloodstream infection due to gram-negative bacilli and only 8 (5.7%) follow-up blood cultures were positive. In contrast, 43 patients (20.8%) of patients with gram-positive cocci BSI had positive follow-up blood cultures. The only factor that predicted a positive follow-up blood culture in patients experiencing bloodstream infection due to gram-negative bacilli was fever at the time of the follow-up blood cultures. Other risk factors examined included whether the patient was receiving antibiotics, the presence of a central venous catheter or urinary catheter, neutropenia, HIV, diabetes, end-stage renal disease on hemodialysis, cirrhosis, ICU care, and mortality. Thus, 17 follow-up blood cultures had to be obtained in patients with gram-negative bacilli BSI in order to define one person with persistent bacteremia.
The authors concluded that routine follow-up blood cultures in patients with gram-negative bacilli bloodstream infection has little value and probably results in added costs and inappropriate use of antibiotics.
For those interested in the topic, another recent study showing that repeat blood cultures are generally unnecessary in patients with gram-negative bacilli bacteremia is Wiggers JB, at al. BMC Infectious Diseases 16:286 (2016).
Along a similar thought line related to misuse of blood cultures – what data supports the common practice of starting the “antibiotic clock” when repeat blood cultures are sterile? To the best of my knowledge, there is very little information to support this common clinical practice. I think in most instances, even in S aureus BSI, this dogmatic practice results in prolonging antibiotic course duration by a few days with associated increases in cost, toxicity, and emergence of resistance with very little demonstrated benefit to the patient.
Content courtesy Dr. Mark Rupp MD.
 There are hundreds of homeless youth in Omaha. Some of them have been emotionally, physically, or sexually abused, making it unsafe for them to return home, while others are facing health, mental health, or substance abuse issues.
There are hundreds of homeless youth in Omaha. Some of them have been emotionally, physically, or sexually abused, making it unsafe for them to return home, while others are facing health, mental health, or substance abuse issues. 
 The successful applicant will also participate in the clinical, teaching, and research programs of the Infectious Diseases Division – a vibrant and growing division made up of
The successful applicant will also participate in the clinical, teaching, and research programs of the Infectious Diseases Division – a vibrant and growing division made up of  Dr. Alison Freifeld has been invited to speak at #IDWeek2018 on new developments in the management of cancer patients, and she is on the steering committee for the American Council on Education (ACE) program at UNMC: goal is to internationalize our campus/curriculum/student body. This program is mandated by the Chancellor and reflects UNMC’s commitment to expanding our efforts in international engagement and global health education and research.
Dr. Alison Freifeld has been invited to speak at #IDWeek2018 on new developments in the management of cancer patients, and she is on the steering committee for the American Council on Education (ACE) program at UNMC: goal is to internationalize our campus/curriculum/student body. This program is mandated by the Chancellor and reflects UNMC’s commitment to expanding our efforts in international engagement and global health education and research. Dr. Jasmine Marcelin was recently co-recipient of the award for Outstanding multi-site Quality Improvement Project for 2017 – Mayo Clinic Quality Review Board {Project: Management of Febrile Neutropenia (MOFN), completed as a fellow with Drs. Jack O’Horo and Omar Abu Saleh}. Dr. Marcelin also co-authored recently published papers about
Dr. Jasmine Marcelin was recently co-recipient of the award for Outstanding multi-site Quality Improvement Project for 2017 – Mayo Clinic Quality Review Board {Project: Management of Febrile Neutropenia (MOFN), completed as a fellow with Drs. Jack O’Horo and Omar Abu Saleh}. Dr. Marcelin also co-authored recently published papers about  Dr. Susan Swindells was recently highlighted in ground-breaking research likely to change the paradigm of latent TB treatment in persons living with HIV; presented at #CROI2018:
Dr. Susan Swindells was recently highlighted in ground-breaking research likely to change the paradigm of latent TB treatment in persons living with HIV; presented at #CROI2018: 
 Dr. Sara Bares‘ academic interests include medical education and research about persons living with HIV. Dr. Bares’ recent publications include a paper in the Journal of Women’s Health demonstrating that
Dr. Sara Bares‘ academic interests include medical education and research about persons living with HIV. Dr. Bares’ recent publications include a paper in the Journal of Women’s Health demonstrating that


 Dr. James Lawler (former White House Homeland Security Council biodefense policy director) was recently called upon to share his expertise pertaining to Biosecurity at the
Dr. James Lawler (former White House Homeland Security Council biodefense policy director) was recently called upon to share his expertise pertaining to Biosecurity at the  IBA is a humanized long-acting IgG4 monoclonal antibody that prevents attachment of the HIV-1 molecule to CD4+ T cells by changing the conformation of the CD4+ T cell receptor while preserving the function of the cell. These functions
IBA is a humanized long-acting IgG4 monoclonal antibody that prevents attachment of the HIV-1 molecule to CD4+ T cells by changing the conformation of the CD4+ T cell receptor while preserving the function of the cell. These functions 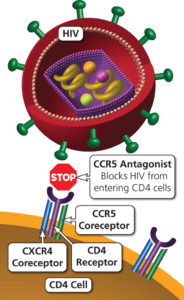




Recent Comments