Two student interest groups, the Infectious Diseases Interest Group and and the Student Alliance for Global Health, collaborated to host a presentation by Dr. Ali Khan, Dean of the College of Public Health and former director for the Office of Public Health Preparedness and Response at the CDC. His professional endeavors have focused on emerging infectious diseases, bioterrorism, and global health security.
The meeting was held in October and had an excellent turnout with close to 60 attendees including students from the College of Medicine, College of Public Health, Pharmacy, and Physicians Assistants.
Dr. Khan spent the first bit of the meeting sharing about how he became interested and involved with infectious diseases and epidemiology, starting with his schooling in Brooklyn for both undergraduate studies and medical school. He told us about his early exposures to epidemiology with the National Center for Infectious Disease and his eventual involvement with the CDC. Throughout his presentation, Dr. Khan emphasized how influential mentors were for advice and motivation in his career. He encouraged all of the students to both ensure they find great mentors to learn from as well as engage in mentoring relationships with younger students.
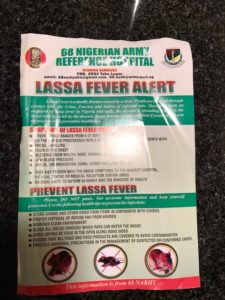
Next Dr. Khan shared several interesting details about some of the more recent epidemics, including the 2014 Ebola outbreak and the 2001 anthrax attacks. Of particular interest, during the Ebola outbreak, was the unique need to carefully understand cultural practices and learn how to educate communities about how to prevent disease spread. He explained how many cases of Ebola were contracted through contact with diseased persons and how funeral practices in the area were contributing to the spread.
A curious detail about the anthrax outbreak came down to the design of envelopes and how mail sorting facilities work! Dr. Khan explained that because letters are sorted with a machine that essentially clamps down on letters to read barcodes, the envelopes have gaps incorporated into how they seal so that air can escape during the sorting process. However, this design caused anthrax spores to be flung all around mail sorting facilities during the outbreak and he explained how this created a unique challenge for public health agencies.
The time was then opened up for questions from the students which Dr. Khan gladly answered with enthusiasm! Overall, the students were inspired by his talk and found his stories fascinating.
Content courtesy of Jonathan Seaman and the IDIG at UNMC.










Recent Comments