 This morning members of our UNMC ID division had the opportunity to have breakfast with the CEO of the Infectious Diseases Society of America (IDSA), Chris Busky, CAE. Though it was early in the morning, our fellows and several faculty made an appearance at the breakfast, where we listened to a short presentation by Mr. Busky, followed by an informal question-and-answer session discussing issues that affect us all as Infectious Diseases physicians. Below is an account of our discussions.
This morning members of our UNMC ID division had the opportunity to have breakfast with the CEO of the Infectious Diseases Society of America (IDSA), Chris Busky, CAE. Though it was early in the morning, our fellows and several faculty made an appearance at the breakfast, where we listened to a short presentation by Mr. Busky, followed by an informal question-and-answer session discussing issues that affect us all as Infectious Diseases physicians. Below is an account of our discussions.
In his presentation, Mr. Busky discussed the strategic priorities of IDSA:
 Strategic Priority 1: Promote the value of the Infectious Diseases Physician/HIV Specialist
Strategic Priority 1: Promote the value of the Infectious Diseases Physician/HIV Specialist
IDSA is committed to spending time and resources to communicate the value of our specialty, and help ID physicians communicate this value to the key stakeholders, including hospital administrators, payers and policy makers. This involves a strategic redefining of our brand and their messaging campaign. They have created a “Value of Infectious Diseases Specialists” toolkit which includes resources for leading Antimicrobial Stewardship Programs. Additionally, they recently produced the largest Infectious Diseases Compensation survey in history with a record 2500 responses (compared to other surveys that only included a paltry single digit percentage of ID physicians) to provide better compensation data for IDSA members. One of our fellows brought up a great point: can we add value to the Infectious Diseases Physician by including access to training for minimally invasive procedures, through point-of-care ultrasound? Think – abscess drainage, paracentesis, thoracentesis, line placement etc… Many non-proceduralists perform these kinds of tests in community hospitals, why not ID physicians? Could this be an opportunity for diagnostic stewardship? The answer to this is unclear, but there may be interest in this as many ID fellow candidates are considering ID-Critical care for this reason.
Strategic Priority 2: Attract the Best and Brightest to ID/HIV
Acknowledging that (a) medical students start to decide on broad scope of specialty (Internal Medicine vs non-Internal Medicine) by their second year of medical school, and (b) Internal Medicine residents decide on subspecialty fellowship interests by their second year of residency, IDSA is increasing efforts to attract medical students and residents to our field. The society now has over 1000 resident/medical student members, and several ID interest groups directly affiliated with IDSA. The society acknowledges the need to continually engage these students/residents well into their training, so that they remain interested in Infectious Diseases when the time comes to pick their specialty. Additionally, IDSA will be piloting a new leadership institute program in 2019. This program will provide an opportunity to create a blended curriculum involving professionals to describe leadership/business core competencies tailored specifically to infectious diseases as a specialty, to promote advancement of ID physicians in leadership positions throughout their careers.
Strategic Priority 3: Promote Leadership in Antimicrobial Resistance and Stewardship
 Society journals have recently released several publications outlining the need for Infectious Disease Leadership in Antimicrobial Stewardship Programs (which ties into the priority of promoting ID Physician value). Acknowledging that these programs are needed (perhaps even more critically so) in smaller communities with limited resources and worldwide, IDSA is actively exploring how to utilize Tele-Stewardship programs nationally and internationally in combination with appropriate compensation models. This tele-health program for Antimicrobial Stewardship is also applicable for long-term health care facilities. Our own Dr. M Salman Ashraf is also exploring this in Nebraska and has collaborated with the CDC and Nebraska Department of Health to create the Nebraska Antimicrobial Stewardship Assessment and Promotion Program (ASAP). Additionally, IDSA has piloted the Antimicrobial Stewardship Centers of Excellence Program to”promote excellence in optimizing antimicrobial use and combating antimicrobial resistance (AMR) by identifying institutions that effectively demonstrate these activities“. Finally, as part of promoting leadership in this area, IDSA is developing an Antimicrobial Stewardship curriculum for fellowship programs, including basic and advanced curricula that should be available for free to ID program directors and fellows later this year.
Society journals have recently released several publications outlining the need for Infectious Disease Leadership in Antimicrobial Stewardship Programs (which ties into the priority of promoting ID Physician value). Acknowledging that these programs are needed (perhaps even more critically so) in smaller communities with limited resources and worldwide, IDSA is actively exploring how to utilize Tele-Stewardship programs nationally and internationally in combination with appropriate compensation models. This tele-health program for Antimicrobial Stewardship is also applicable for long-term health care facilities. Our own Dr. M Salman Ashraf is also exploring this in Nebraska and has collaborated with the CDC and Nebraska Department of Health to create the Nebraska Antimicrobial Stewardship Assessment and Promotion Program (ASAP). Additionally, IDSA has piloted the Antimicrobial Stewardship Centers of Excellence Program to”promote excellence in optimizing antimicrobial use and combating antimicrobial resistance (AMR) by identifying institutions that effectively demonstrate these activities“. Finally, as part of promoting leadership in this area, IDSA is developing an Antimicrobial Stewardship curriculum for fellowship programs, including basic and advanced curricula that should be available for free to ID program directors and fellows later this year.
Strategic Priority 4: Produce Relevant Guidelines
IDSA is committed to producing high-quality guidelines, using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach to standardize and improve quality of guidelines. Guideline committees will work with an ID physician guideline specialist and methodologist to have more streamlined and consistent development guidelines that address relevant clinical needs. They have also committed to rapid turn-around, high-level updates of guidelines and better coordination with international society guidelines.
Strategic Priorities 5 & 6: Promote ID/HIV Research, and Advocate for Public Health Funding in ID/HIV
 IDSA has been a strong funding advocate. They advocate for funds through the National Institute of Allergy and Infectious Diseases (NIAID), Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA). Additionally, they advocate for Global Health through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), and United States Agency for International Development (USAID). IDSA has several ID/HIV funding programs for which members are eligible. Tied to the priority of attracting the Best and Brightest, to promote research in HIV/ID, IDSA has been funding the Medical Scholars Program. Finally, membership to the HIV Medicine Association is included in IDSA membership, and this sub-society is dedicated to promoting quality in HIV care, directing major HIV-related policies and guidelines.
IDSA has been a strong funding advocate. They advocate for funds through the National Institute of Allergy and Infectious Diseases (NIAID), Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA). Additionally, they advocate for Global Health through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), and United States Agency for International Development (USAID). IDSA has several ID/HIV funding programs for which members are eligible. Tied to the priority of attracting the Best and Brightest, to promote research in HIV/ID, IDSA has been funding the Medical Scholars Program. Finally, membership to the HIV Medicine Association is included in IDSA membership, and this sub-society is dedicated to promoting quality in HIV care, directing major HIV-related policies and guidelines.
Member Engagement
 IDSA has >11,000 members in 100+ countries across 6 continents, and the society is constantly working on transforming their brand. They will be moving towards more personalized engagement, featuring stories of physician members, fellows, resident/students interested in ID. The annual conference has been improving in popularity each year,largely due to improved content, more opportunities for interaction and new features (ID Bug Bowl was a blast!). IDSA is being more deliberate about creating personal connections, engaging dynamics, relevant content and opportunities for networking with smaller, more interactive sessions to transform the conference.
IDSA has >11,000 members in 100+ countries across 6 continents, and the society is constantly working on transforming their brand. They will be moving towards more personalized engagement, featuring stories of physician members, fellows, resident/students interested in ID. The annual conference has been improving in popularity each year,largely due to improved content, more opportunities for interaction and new features (ID Bug Bowl was a blast!). IDSA is being more deliberate about creating personal connections, engaging dynamics, relevant content and opportunities for networking with smaller, more interactive sessions to transform the conference.
 IDWeek 2018 will be in San Francisco October 3-7 (UNMC_ID will be there!). There are also additional opportunities for fellows to get involved, and Open Forum Infectious Diseases is an opportunity for ID fellows to submit their work for publication. There are clinical and research meetings for fellows occurring in April and June 2018 respectively. IDSA encourages active membership engagement, and the society is committed to providing volunteering roles for all who want to be involved-advocacy, website content, media core (be a content expert), journal club, education, mentorship etc. Regarding engagement in political advocacy, the society had record engagement (>4000) from members in 2017 with face to face meetings, action alerts, member visits in local communities. Mr. Busky emphasized that the society’s role in advocacy is never complete – engagement with congress is ongoing, building and strengthening relationships on Capitol Hill to advance the priorities of the society representing its individual physician members. He encouraged physician members to be a consistent voice reaching out to Congressional representatives with the message to prioritize ID/HIV concerns.
IDWeek 2018 will be in San Francisco October 3-7 (UNMC_ID will be there!). There are also additional opportunities for fellows to get involved, and Open Forum Infectious Diseases is an opportunity for ID fellows to submit their work for publication. There are clinical and research meetings for fellows occurring in April and June 2018 respectively. IDSA encourages active membership engagement, and the society is committed to providing volunteering roles for all who want to be involved-advocacy, website content, media core (be a content expert), journal club, education, mentorship etc. Regarding engagement in political advocacy, the society had record engagement (>4000) from members in 2017 with face to face meetings, action alerts, member visits in local communities. Mr. Busky emphasized that the society’s role in advocacy is never complete – engagement with congress is ongoing, building and strengthening relationships on Capitol Hill to advance the priorities of the society representing its individual physician members. He encouraged physician members to be a consistent voice reaching out to Congressional representatives with the message to prioritize ID/HIV concerns.
Burnout/Stress
 Mr. Busky wanted to know what we are doing to address stress/burnout here. Our general ID service is our busiest clinical inpatient service. Acknowledging this, our Division Chief Dr. Mark Rupp has already made plans to split this service into two. This will significantly reduce the patient census and make a difference in reducing stress. Of course, time spent documenting in the EMR (universal problem for all medical specialties) contributes to stress/burnout, when physicians are spending 2-3 hrs after care is provided to document in EMR. The group felt that one of the biggest contributors to burnout/stress in our specialty is the struggle with with communicating value of ID outside our division – many ID physicians find themselves engaged in several different activities to “prove their worth”, compared to some proceduralist specialties which may be able to focus more on what they actually trained to do for the same (but usually higher) compensation. In the same thread, we discussed how to communicate the value of ID sub specialties such as Oncology-ID, Ortho-ID, or Transplant-ID to the related medical specialties in promoting this niche care. Mr. Busky shared that IDSA is part of the “Cognitive Care Alliance” of specialties, collectively working towards advocating for value of these cognitive specialties.
Mr. Busky wanted to know what we are doing to address stress/burnout here. Our general ID service is our busiest clinical inpatient service. Acknowledging this, our Division Chief Dr. Mark Rupp has already made plans to split this service into two. This will significantly reduce the patient census and make a difference in reducing stress. Of course, time spent documenting in the EMR (universal problem for all medical specialties) contributes to stress/burnout, when physicians are spending 2-3 hrs after care is provided to document in EMR. The group felt that one of the biggest contributors to burnout/stress in our specialty is the struggle with with communicating value of ID outside our division – many ID physicians find themselves engaged in several different activities to “prove their worth”, compared to some proceduralist specialties which may be able to focus more on what they actually trained to do for the same (but usually higher) compensation. In the same thread, we discussed how to communicate the value of ID sub specialties such as Oncology-ID, Ortho-ID, or Transplant-ID to the related medical specialties in promoting this niche care. Mr. Busky shared that IDSA is part of the “Cognitive Care Alliance” of specialties, collectively working towards advocating for value of these cognitive specialties.
Diversity
 IDSA acknowledges there are gender and racial disparities within our ID workforce. Their first goal was to evaluate it to see what the gaps are as described in this publication. Now that the extent of the gap has been identified, IDSA has committed to integrating principles of Diversity, Inclusion & Equity into the core values of the society. The IDSA board will go through training to define these principles and model to the society, with the goal of not only recruiting more women and under-represented minorities, but improving visibility this commitment to membership by ensuring that women and People of Color are represented on leadership committees, award recipients, ID week speakers and society representatives. Additionally, the society aims to diversify the membership and leadership geographically, to ensure that there is representation of more individuals from Midwest/mountain regions. Finally, they recognize that there is a need for more clinical representation on leadership committees and are working to diversify their boards in this way also.
IDSA acknowledges there are gender and racial disparities within our ID workforce. Their first goal was to evaluate it to see what the gaps are as described in this publication. Now that the extent of the gap has been identified, IDSA has committed to integrating principles of Diversity, Inclusion & Equity into the core values of the society. The IDSA board will go through training to define these principles and model to the society, with the goal of not only recruiting more women and under-represented minorities, but improving visibility this commitment to membership by ensuring that women and People of Color are represented on leadership committees, award recipients, ID week speakers and society representatives. Additionally, the society aims to diversify the membership and leadership geographically, to ensure that there is representation of more individuals from Midwest/mountain regions. Finally, they recognize that there is a need for more clinical representation on leadership committees and are working to diversify their boards in this way also.
Today, Mr. Busky came to us and by just having a conversation with us, showed us that IDSA is working for us, dedicated to personalizing its connection with members and pursuing our common interests. Thank you for sharing!
 Dr. Jasmine Marcelin presented a study in ID Journal Club recently that applied an antimicrobial stewardship intervention to this patient population.
Dr. Jasmine Marcelin presented a study in ID Journal Club recently that applied an antimicrobial stewardship intervention to this patient population.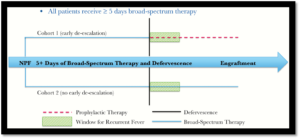 This was a single-center retrospective cohort study looking at allogeneic hematopoietic stem cell transplant (HSCT) patients with febrile neutropenia (who had defervesced and were clinically stable) who were de-escalated to neutropenic prophylaxis after 5 days (cohort 1) vs those who were continued on broad-spectrum therapy until engraftment (cohort 2). The study included 120 patients, with 46 in cohort 1 and 74 in cohort 2. The question: if patients are de-escalated after 5 days, are they more likely to have recurrent fever?
This was a single-center retrospective cohort study looking at allogeneic hematopoietic stem cell transplant (HSCT) patients with febrile neutropenia (who had defervesced and were clinically stable) who were de-escalated to neutropenic prophylaxis after 5 days (cohort 1) vs those who were continued on broad-spectrum therapy until engraftment (cohort 2). The study included 120 patients, with 46 in cohort 1 and 74 in cohort 2. The question: if patients are de-escalated after 5 days, are they more likely to have recurrent fever?



 This morning members of our UNMC ID division had the opportunity to have breakfast with the CEO of the
This morning members of our UNMC ID division had the opportunity to have breakfast with the CEO of the  Strategic Priority 1: Promote the value of the Infectious Diseases Physician/HIV Specialist
Strategic Priority 1: Promote the value of the Infectious Diseases Physician/HIV Specialist Society journals have recently released several publications outlining the need for Infectious Disease Leadership in Antimicrobial Stewardship Programs (which ties into the priority of promoting ID Physician value). Acknowledging that these programs are needed (perhaps even more critically so) in smaller communities with limited resources and worldwide, IDSA is actively exploring how to utilize Tele-Stewardship programs nationally and internationally in combination with appropriate compensation models. This tele-health program for Antimicrobial Stewardship is also applicable for long-term health care facilities. Our own Dr. M Salman Ashraf is also exploring this in Nebraska and has collaborated with the CDC and Nebraska Department of Health to create the
Society journals have recently released several publications outlining the need for Infectious Disease Leadership in Antimicrobial Stewardship Programs (which ties into the priority of promoting ID Physician value). Acknowledging that these programs are needed (perhaps even more critically so) in smaller communities with limited resources and worldwide, IDSA is actively exploring how to utilize Tele-Stewardship programs nationally and internationally in combination with appropriate compensation models. This tele-health program for Antimicrobial Stewardship is also applicable for long-term health care facilities. Our own Dr. M Salman Ashraf is also exploring this in Nebraska and has collaborated with the CDC and Nebraska Department of Health to create the  IDSA has >11,000 members in 100+ countries across 6 continents, and the society is constantly working on transforming their brand. They will be moving towards more personalized engagement, featuring stories of physician members, fellows, resident/students interested in ID. The annual conference has been improving in popularity each year,largely due to improved content, more opportunities for interaction and new features (ID Bug Bowl was a blast!). IDSA is being more deliberate about creating personal connections, engaging dynamics, relevant content and opportunities for networking with smaller, more interactive sessions to transform the conference.
IDSA has >11,000 members in 100+ countries across 6 continents, and the society is constantly working on transforming their brand. They will be moving towards more personalized engagement, featuring stories of physician members, fellows, resident/students interested in ID. The annual conference has been improving in popularity each year,largely due to improved content, more opportunities for interaction and new features (ID Bug Bowl was a blast!). IDSA is being more deliberate about creating personal connections, engaging dynamics, relevant content and opportunities for networking with smaller, more interactive sessions to transform the conference.
 Mr. Busky wanted to know what we are doing to address stress/burnout here. Our general ID service is our busiest clinical inpatient service. Acknowledging this, our Division Chief Dr. Mark Rupp has already made plans to split this service into two. This will significantly reduce the patient census and make a difference in reducing stress. Of course, time spent documenting in the EMR (universal problem for all medical specialties) contributes to stress/burnout, when physicians are spending 2-3 hrs after care is provided to document in EMR. The group felt that one of the biggest contributors to burnout/stress in our specialty is the struggle with with communicating value of ID outside our division – many ID physicians find themselves engaged in several different activities to “prove their worth”, compared to some proceduralist specialties which may be able to focus more on what they actually trained to do for the same (but usually higher) compensation. In the same thread, we discussed how to communicate the value of ID sub specialties such as Oncology-ID, Ortho-ID, or Transplant-ID to the related medical specialties in promoting this niche care. Mr. Busky shared that IDSA is part of the “Cognitive Care Alliance” of specialties, collectively working towards advocating for value of these cognitive specialties.
Mr. Busky wanted to know what we are doing to address stress/burnout here. Our general ID service is our busiest clinical inpatient service. Acknowledging this, our Division Chief Dr. Mark Rupp has already made plans to split this service into two. This will significantly reduce the patient census and make a difference in reducing stress. Of course, time spent documenting in the EMR (universal problem for all medical specialties) contributes to stress/burnout, when physicians are spending 2-3 hrs after care is provided to document in EMR. The group felt that one of the biggest contributors to burnout/stress in our specialty is the struggle with with communicating value of ID outside our division – many ID physicians find themselves engaged in several different activities to “prove their worth”, compared to some proceduralist specialties which may be able to focus more on what they actually trained to do for the same (but usually higher) compensation. In the same thread, we discussed how to communicate the value of ID sub specialties such as Oncology-ID, Ortho-ID, or Transplant-ID to the related medical specialties in promoting this niche care. Mr. Busky shared that IDSA is part of the “Cognitive Care Alliance” of specialties, collectively working towards advocating for value of these cognitive specialties. IDSA acknowledges there are gender and racial disparities within our ID workforce. Their first goal was to evaluate it to see what the gaps are as described in
IDSA acknowledges there are gender and racial disparities within our ID workforce. Their first goal was to evaluate it to see what the gaps are as described in 




Recent Comments