The Nebraska Infectious Diseases Society (NIDS) annual meeting is this Friday, August 23rd. If you still need to register, check out our previous posts on the meeting and the keynote address for more information.
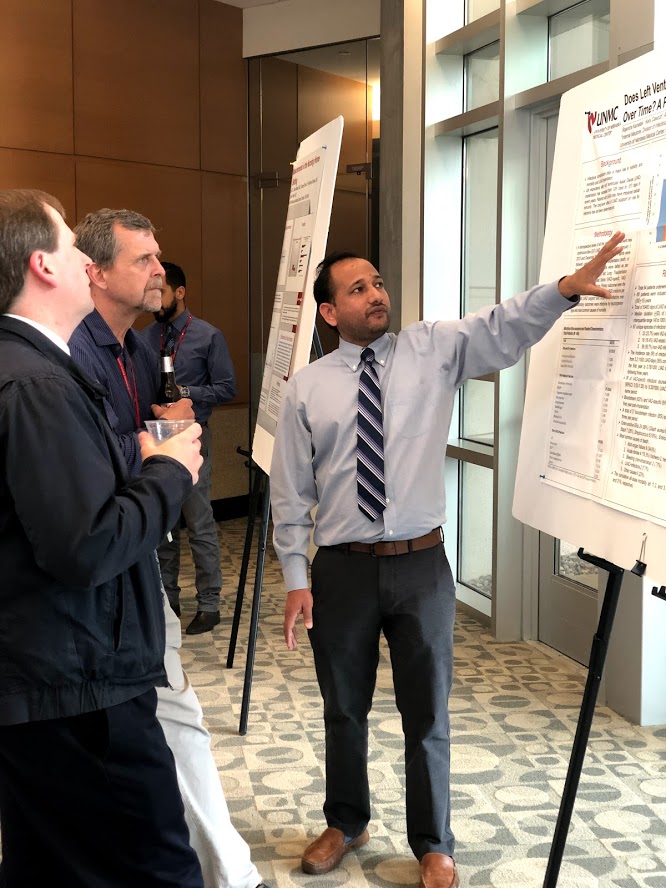
One of the most anticipated events held during the meeting is the poster session, which continues to grow each year and features fascinating cases and novel research, most of which is led by trainees, residents, and fellows. This year, the top abstracts in each category will also be presented orally. A huge congratulations to our top abstract winners: John Glassmann, who will present Data-driven strategies towards case management utilizing Tableau dashboard reporting and automation from the research category, and Sarah Uhm & Kari Havyer, who will present their clinical vignette Extrapulmonary Osteoarticular and CNS Tuberculosis: A Case Report. In addition to these talks, dozens of other fascinating projects will be presented as part of the poster session. Read on below for a digest of presenters to help plan your day.
Research Category:
| Poster # | Project Title | Presenting Author |
| 2 | A Quality Improvement Project to Improve Utilization of Sputum Cultures in Hospitalized Patients with Pneumonia | Jennifer Zimmerman |
| 17 | Inconsistent Participant Demographic Reporting in Published Antibiotic Clinical Trials Targeting Multidrug-Resistant Gram-Negative Organisms | Dr. Evangeline Green |
| 22 | Medicaid Insurance Expansion and its Association with HIV Outcomes in Nebraska, USA: An Observational Prospective Cohort Study | Emmanuel Essam |
| 23 | Urine testing in the emergency department: an analysis of the frequency of inappropriate testing and an economic analysis | Alex Larson |
| 24 | A retrospective review of health disparities in achieving sustained virologic response in chronic Hepatitis C infection: A single center experience | Eileen Leach |
| 28 | Evaluating the Effects of Hepatitis C Treatment With Direct-Acting Antivirals on Glycemic Control in Patients With Diabetes Mellitus | Ricky Rana |
| 29 | Association Between Adherence Barriers and Pharmacy Refill History in People with HIV after Medicaid Expansion in Nebraska: An observational retrospective cohort study. | Elizabeth Amato-Hanner |
| 30 | Data-driven strategies towards case management utilizing Tableau dashboard reporting and automation | John Glassman |
| 33 | Duration of Daptomycin and Ceftaroline Dual Therapy in Salvage Methicillin Resistant Staphylococcus aureus(MRSA) Bacteremia Prior to Monotherapy De-escalation | Dr. Josh Lechner |
Clinical Vignettes Category:
| Poster # | Project Title | Presenting Author |
| 3 | A Fungal Tracheitis and Epiglottitis with Bacterial Superinfection in an Immunocompromised Teenager: A Long Road to Confirmation | Haley DeWitt |
| 4 | Disseminated Mycobacterium Bovis with Prosthetic Joint Infection | Madeline Helm |
| 5 | A Picture Worth a Thousand Words: Incidentally Diagnosed Neurocysticercosis and Barriers to its Treatment | Dr. Emily Dyer |
| 7 | A rare case of idiopathic granulomatous mastitis with Corynebacterium kroppenstedtii infection in the setting of pregnancy and erythema nodosum | Lauren Ziegenbein |
| 8 | Syphilis-Related Glomerulopathy: A Rare Presentation of a Common Disease | Shalmali Mirajkar |
| 9 | Veillonella parvula Bacteremia in a Diabetic Patient with Osteomyelitis and Soft Tissue Infection Linked to Onychophagia | Emily Ehsan |
| 10 | The Diagnostic Dilemma of an Atypical Bacterial Ventriculoperitoneal Shunt Infection in an Immunocompetent Child | Dr. Christian Clodfelder |
| 11 | Disseminated Mycobacterium bovis with severe thrombocytopenia during treatment: A diagnostic and therapeutic dilemma | Lauren Crockett |
| 12 | Not quite Bacillus. Not quite an Aneurysm. Navigating diagnostic challenges of a rare pseudoaneurysm infection. | Jacob Owens |
| 13 | Extrapulmonary Osteoarticular and CNS Tuberculosis: A Case Report | Sarah Uhm &, Kari Havyer |
| 14 | A Case of Severe Mucositis Following Mycoplasma Infection | Dr. Abby Wolfe |
| 15 | Blastomyces dermatitidis Cervical Spine Osteomyelitis and Paraspinal Abscess in Nebraska | Ellie Staab |
| 16 | Cutaneous Mycobacterium abscessus infection in an immunocompetent teenage female | Matthew Muellner |
| 19 | 4 weeks of dyspnea in immunocompromised woman; presenting symptom of disseminated Histoplasmosis Capsulatum | Dr. Cristina Torres |
| 20 | Breakthrough osteomyelitis with opportunistic canine oral flora in an immunocompromised patient | Ryan Chapman |
| 21 | Mycolicibacterium smegmatis: a rare cause of sternal osteomyelitis | Jose Ortega |
| 25 | Fusobacterium nucleatum mimicking lung cancer: A case report | Sarah Maki |
| 26 | Rare Case of Ignatzschineria larvae Bacteremia in a Myiatic Wound Infection: A Case Report | Dr. Nicholas Mielke |
| 31 | Unrecognized Complications: The Uncommon Occurrence of PJP Pneumonia in lung cancer on Durvalumab | Dr. Narmada Lavu |










Recent Comments