 Bellevue Medical Center (BMC) is a community hospital campus of Nebraska Medicine. In 2017, our Nebraska Medicine Antimicrobial Stewardship Program expanded to include BMC with the expansion of our ASP expertise at our main campus. Danny Schroeder, a pharmacist at BMC, was recruited to lead the stewardship activities on that campus, with expertise provided by Dr. Jasmine Marcelin. In celebrating #AntibioticAwarenessWeek, Danny shares his thoughts on community stewardship. Danny can be found on Twitter at @dkschroePharmD
Bellevue Medical Center (BMC) is a community hospital campus of Nebraska Medicine. In 2017, our Nebraska Medicine Antimicrobial Stewardship Program expanded to include BMC with the expansion of our ASP expertise at our main campus. Danny Schroeder, a pharmacist at BMC, was recruited to lead the stewardship activities on that campus, with expertise provided by Dr. Jasmine Marcelin. In celebrating #AntibioticAwarenessWeek, Danny shares his thoughts on community stewardship. Danny can be found on Twitter at @dkschroePharmD
Antimicrobial stewardship is becoming more important every day. The CDC just released Antibiotic Resistance Threats in the United States, 2019 in which the Director of the CDC warns that we are now in the post antibiotic era. Antimicrobial stewardship needs to be a global effort, and everyone in every health care setting can help.
In a recent JAMA article, the feasibility of antimicrobial stewardship interventions in community hospitals was evaluated. Local pharmacists were trained on how to address common stewardship questions and anticipated arguments. They utilized two different mechanisms: pre-authorization of antimicrobials (PA) and post prescription review of antimicrobials (PPR). Pharmacists received bimonthly feedback from the study site during the trial period. They found that while feasible, the mechanisms used in the study did not result in major improvements in antibiotic use. PA was found to be ineffective, while PPR resulted in a statistically significant reduction in antibiotic use, however, the absolute reduction in use was only about 5%.
At the Bellevue Medical Center, I employ the PPR mechanism when performing antimicrobial stewardship. This leads to more discussions with clinicians and allows me to create stronger relationships with them. With stronger relationships comes more trust that my recommendations are appropriate and that they follow guideline-based therapy. To aide me in my stewardship endeavors, I have the privilege to discuss complex patients with an ID expert at Nebraska Medicine, Dr. Jasmine Marcelin, twice a week. I learn something new almost every week and am able to take that knowledge forward to continue to improve my stewardship practice. In addition, I can contact expert antimicrobial stewardship pharmacists at Nebraska Medicine for assistance if needed.
Having local expertise and leadership support is something the pharmacists did not have in the JAMA article mentioned above. The pharmacists also only received bimonthly feedback while I get assistance twice a week. I believe stewardship activities supported by ID experts is a crucial step a successful stewardship program at a community hospital where pharmacy staff may not be formally trained in infectious disease and antimicrobial stewardship. Having this expertise readily available is invaluable. It increases my confidence with my recommendations and I know the interventions I make are making a positive impact on patient care.
One last item I would like to mention is #IDTwitter. I was reluctant to join Twitter for quite some time, thinking it was another “time-suck” like Facebook. I was very wrong. I have learned many great pieces of information from multiple ID experts in the US and around the world on Twitter. In community hospital settings where ID expertise may not be readily available, knowing where to find information is key. #IDTwitter is a great place to start as there are a multitude of ID experts sharing their pearls of wisdom and analysis of newly released studies every day.
We are in the post antibiotic era. No matter which healthcare setting you are a part of, you can help. Join me and the countless others in the US and around the world in the fight against antimicrobial resistance. #BeAntibiocisAware.
 In recognition of this annual observance, Governor Pete Ricketts signed a proclamation on November 4, 2009 in the State Capitol designating November 18 to 24 Antibiotic Awareness Week in Nebraska. Dr. Maureen Tierney, the head of the
In recognition of this annual observance, Governor Pete Ricketts signed a proclamation on November 4, 2009 in the State Capitol designating November 18 to 24 Antibiotic Awareness Week in Nebraska. Dr. Maureen Tierney, the head of the 
 Survey Link: (
Survey Link: (
 This year, the UNMC HIV Update for Care Providers and Educators on October 10, 2019 brought approximately 100 attendees to Omaha again to learn about new drugs, management approaches, and patient experiences with HIV. The CME conference was funded by the Nebraska AIDS Education & Training Center (AETC), [a local partner of the Midwest AETC], and the Nebraska Department of Health & Human Services. One of our medical students, Brandon Lew, attended and shared his thoughts about the conference here.
This year, the UNMC HIV Update for Care Providers and Educators on October 10, 2019 brought approximately 100 attendees to Omaha again to learn about new drugs, management approaches, and patient experiences with HIV. The CME conference was funded by the Nebraska AIDS Education & Training Center (AETC), [a local partner of the Midwest AETC], and the Nebraska Department of Health & Human Services. One of our medical students, Brandon Lew, attended and shared his thoughts about the conference here. 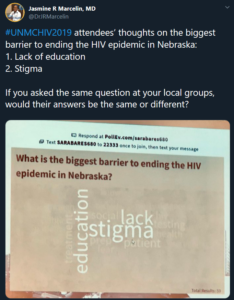 She then turned to the audience and asked what they thought the biggest barrier to ending the HIV epidemic in Nebraska was. Free responses were submitted through our phones and immediately a word cloud was generated using the audience’s answers. This was not only a super cool way of making the presentations interactive and engaging, but also highly impactful seeing professional consensus that 1) lack of education and 2) stigma were major barriers to HIV care.
She then turned to the audience and asked what they thought the biggest barrier to ending the HIV epidemic in Nebraska was. Free responses were submitted through our phones and immediately a word cloud was generated using the audience’s answers. This was not only a super cool way of making the presentations interactive and engaging, but also highly impactful seeing professional consensus that 1) lack of education and 2) stigma were major barriers to HIV care. Dr. Nada Fadul, MD, Precious Davis, MSN, RN, and Tommy Young-Dennis presented on connecting patients in a talk entitled “Meeting Them Where They Are: Strategies to Engage Black MSM in HIV Care and Prevention Services.” Their passion for not just treating, but truly caring for patients and their lives was striking. They advised to engage the patient and learn about their struggles, “keep it real,” and be mindful your own of verbal and nonverbal communication. Interestingly there were also talks which did not centrally focus on HIV, including presentations on current trends in illegal drug use in Omaha, and how to have a dialogue with refugee populations living around Omaha. These patient focused discussions and locally driven information were especially impactful because they were not jargon filled lectures, but rather topical information on subjects that are important for patient care.
Dr. Nada Fadul, MD, Precious Davis, MSN, RN, and Tommy Young-Dennis presented on connecting patients in a talk entitled “Meeting Them Where They Are: Strategies to Engage Black MSM in HIV Care and Prevention Services.” Their passion for not just treating, but truly caring for patients and their lives was striking. They advised to engage the patient and learn about their struggles, “keep it real,” and be mindful your own of verbal and nonverbal communication. Interestingly there were also talks which did not centrally focus on HIV, including presentations on current trends in illegal drug use in Omaha, and how to have a dialogue with refugee populations living around Omaha. These patient focused discussions and locally driven information were especially impactful because they were not jargon filled lectures, but rather topical information on subjects that are important for patient care.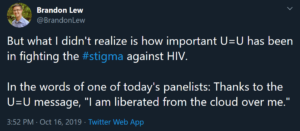

 This year, our ID division was well represented at IDWeek, with several residents and students attending (and presenting) for the first time. One of our third year Internal Medicine/Pediatrics residents interested in Infectious Diseases, Dr. Joe Wang, wrote about his experiences,
This year, our ID division was well represented at IDWeek, with several residents and students attending (and presenting) for the first time. One of our third year Internal Medicine/Pediatrics residents interested in Infectious Diseases, Dr. Joe Wang, wrote about his experiences, 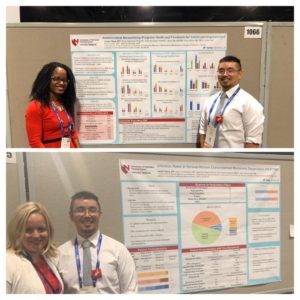




 It was gratifying to see the teams have fun with it. It was such a simple way to have fun at work but raise awareness about the importance of hand hygiene.
It was gratifying to see the teams have fun with it. It was such a simple way to have fun at work but raise awareness about the importance of hand hygiene.
Recent Comments