An October 2018 publication in Critical Care Medicine by Chuang et al details a prospective study of adults in Taiwan, between 2010 -2015, aimed to assess all-cause mortality and rate of bloodstream clearance among patients with vancomycin-resistant enterococci (VRE) treated with daptomycin (bacteriocidal) versus linezolid(bacteriostatic). Patients were treated with conventional daptomycin (6 to < 9 mg/kg actual body weight), high-dose daptomycin(>9 mg/kg) or linezolid (600mg IV Q12 hours). The initial blood culture bacterial load was determined, followed by blood cultures daily for the first 4 days and then twice per week for a total of 2 weeks unless the patient was discharged or therapy discontinued prior to that. Blood cultures were assessed via traditional blood culture methodology and by a real-time quantitative PCR detecting vanA (no vanB documented in cohort).
108 patients were included in the analysis. 63(58.3%) received conventional dose daptomycin, 15 (13.9%) received high-dose daptomycin and 30(27.8%) received linezolid. There was no statistically significant difference between survivors and non-survivors in the initial bacterial load, however, survivors had a statistically significant higher rate of early bacterial clearance (p = 0.02). There was no statistically significant difference in bacterial clearance among those with empiric versus definitive treatment, however clearance was statistically significant in difference among the antimicrobial treatment arms. Early bacterial clearance was faster with high-dose daptomycin(p<0.001) and linezolid(p =0.043) as compared to conventional daptomycin, with no statistically significant difference between high-dose daptomycin and linezolid. A higher PITT bacteremia score and slower clearance of bacteremia were found to be independent predictors of mortality. PCR was more sensitive, and equally as specific, as traditional blood cultures.
The statistically significant differences in rate of bacterial clearance (and associated survivorship) between high-dose daptomycin and linezolid, compared to conventional daptomycin, suggests that higher doses of daptomycin or use of linezolid should be considered in VRE BSIs. Larger studies are needed to validate the results and validated determine clinical impact and optimal dosing.
Of note, the study is limited by smaller sample sizes, no vanB carrying VRE and the inability to report false positive PCRs. A formal RCT would be needed to determine optimal therapy. In addition, the average weight of patients was 60 kg, thus this data cannot be extrapolated necessarily to obese patients. Further studies related to dosing weight and optimal dosing are also warranted.
Content originally written and adapted for the IDSA journal club.
 Both of these studies identify clear targets for antibiotic (and diagnostic) stewardship with respect to SSTIs. Utilization of SXT in cases of impetigo could lead to more monotherapy and reduction of unnecessary “double coverage” antibiotic use; reinforcement of the need for only beta-lactams for non-purulent cellulitis is an important area for improvement; and avoidance of unnecessary blood cultures reduces the need for inappropriate antibiotic therapy for contaminants.
Both of these studies identify clear targets for antibiotic (and diagnostic) stewardship with respect to SSTIs. Utilization of SXT in cases of impetigo could lead to more monotherapy and reduction of unnecessary “double coverage” antibiotic use; reinforcement of the need for only beta-lactams for non-purulent cellulitis is an important area for improvement; and avoidance of unnecessary blood cultures reduces the need for inappropriate antibiotic therapy for contaminants.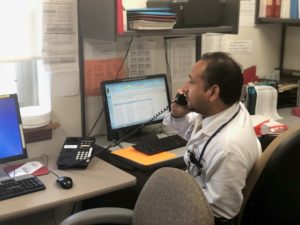 Our antimicrobial stewardship training is concentrated on learning the CDC core elements of antimicrobial stewardship and implementing principles of antimicrobial stewardship in healthcare settings (Inpatient, outpatient, long-term care facility). Fellows actively engage in quality improvement in the infection control and antimicrobial stewardship and also work closely with our Stewardship Pharmacy Coordinator. Learning stewardship core elements present you to principles that can very well be applied to a wide variety of QI efforts. As fellows we are fully integrated into the stewardship team during our rotation, and besides attending key meetings where brainstorming stewardship issues occur and decisions are made, we actively participate in daily telephone audit-and-feedback. This gives us needed practice with communicating with prescribers, troubleshooting common problems and helps us to be better Infectious Disease Doctors. We are also participating in the IDSA Antimicrobial Stewardship Curriculum pilot. In this formal training, our curriculum Directors Drs. Van Schooneveld and Marcelin meet with us regularly for case-studies, role playing and module reviews, where we discuss approaches to handling difficult situations as #Stewies.
Our antimicrobial stewardship training is concentrated on learning the CDC core elements of antimicrobial stewardship and implementing principles of antimicrobial stewardship in healthcare settings (Inpatient, outpatient, long-term care facility). Fellows actively engage in quality improvement in the infection control and antimicrobial stewardship and also work closely with our Stewardship Pharmacy Coordinator. Learning stewardship core elements present you to principles that can very well be applied to a wide variety of QI efforts. As fellows we are fully integrated into the stewardship team during our rotation, and besides attending key meetings where brainstorming stewardship issues occur and decisions are made, we actively participate in daily telephone audit-and-feedback. This gives us needed practice with communicating with prescribers, troubleshooting common problems and helps us to be better Infectious Disease Doctors. We are also participating in the IDSA Antimicrobial Stewardship Curriculum pilot. In this formal training, our curriculum Directors Drs. Van Schooneveld and Marcelin meet with us regularly for case-studies, role playing and module reviews, where we discuss approaches to handling difficult situations as #Stewies. As a part of my stewardship project, I am working on developing an institutional guidance document for antibiotic management of acute rhinosinusitis and pharyngitis in the outpatient setting. My other project is in infection control for the prevention of ventilator-associated events. I also had the opportunity to work with a larger multidisciplinary sepsis group for the development and implementation of institutional sepsis protocol. As a budding Infectious Diseases physician with particular interest in Critical Care Medicine, I know that Antimicrobial Stewardship is essential to any job I take post-fellowship, and I am thrilled to be at an institution that values it so highly.
As a part of my stewardship project, I am working on developing an institutional guidance document for antibiotic management of acute rhinosinusitis and pharyngitis in the outpatient setting. My other project is in infection control for the prevention of ventilator-associated events. I also had the opportunity to work with a larger multidisciplinary sepsis group for the development and implementation of institutional sepsis protocol. As a budding Infectious Diseases physician with particular interest in Critical Care Medicine, I know that Antimicrobial Stewardship is essential to any job I take post-fellowship, and I am thrilled to be at an institution that values it so highly. The highlights of Nebraska ASAP initiative include:
The highlights of Nebraska ASAP initiative include: • Organized the inaugural “Antimicrobial Stewardship Summit” for the state of Nebraska on June 1st 2018 to provide education to ASP program leaders (over 250 healthcare workers attended the summit)
• Organized the inaugural “Antimicrobial Stewardship Summit” for the state of Nebraska on June 1st 2018 to provide education to ASP program leaders (over 250 healthcare workers attended the summit)
 We are also focusing efforts on Outpatient Antimicrobial Stewardship. While this program is still in its nascent stages, in collaboration with
We are also focusing efforts on Outpatient Antimicrobial Stewardship. While this program is still in its nascent stages, in collaboration with 
 The dogs had a moderate interrater reliability with a Cohen’s kappa of 0.52. Both dogs had about 85% specificity of toxigenic C. difficile detection but the German Shepherd’s sensitivity of detection out-sniffed the Border Collie Pointer (92% vs 78% respectively). Positive predictive value for both dogs was <50% and negative predictive value was >95% for both dogs. Interrater variability necessitates individualized dog training; and it is curious that two different species were used – could there be a genetic predisposition for “better” olfactory receptors in certain species?
The dogs had a moderate interrater reliability with a Cohen’s kappa of 0.52. Both dogs had about 85% specificity of toxigenic C. difficile detection but the German Shepherd’s sensitivity of detection out-sniffed the Border Collie Pointer (92% vs 78% respectively). Positive predictive value for both dogs was <50% and negative predictive value was >95% for both dogs. Interrater variability necessitates individualized dog training; and it is curious that two different species were used – could there be a genetic predisposition for “better” olfactory receptors in certain species?
 If two different canine species could not agree on whether or not the stool smelled “diffy”, where does that leave humans, whose olfactory capabilities are thought to be
If two different canine species could not agree on whether or not the stool smelled “diffy”, where does that leave humans, whose olfactory capabilities are thought to be
Recent Comments