Atlanta, GA | October 19–22, 2025
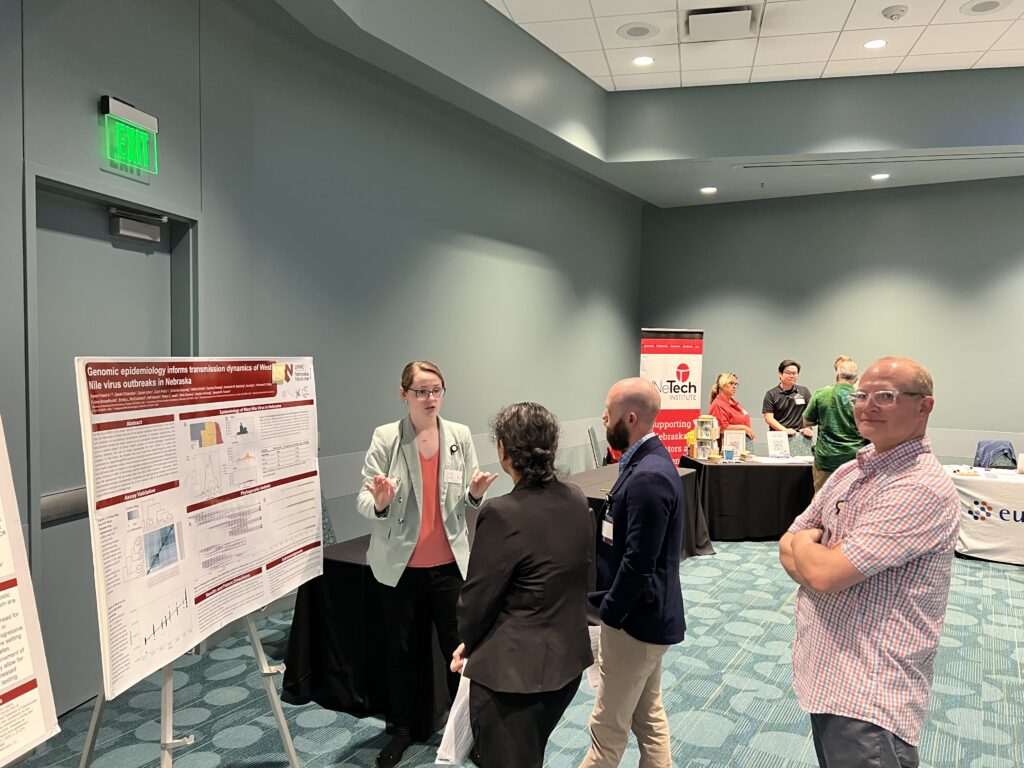
The infectious diseases community is gathering once again for IDWeek 2025, and the University of Nebraska Medical Center (UNMC) Division of Infectious Diseases is proud to be well represented at this premier international conference. With a strong lineup of presentations, posters, and panels, UNMC ID faculty, fellows, and collaborators are showcasing their impactful work across clinical care, research, education, and public health.
Highlights from UNMC ID Presenters
This year’s IDWeek features a diverse array of contributions from UNMC ID members, with 44 presentations by 30 members of our division including several premedical student, medical student, pharmacy student, resident, and fellow, presenters! Click the arrows below to see where to find us in different session types at IDWeek:
Session Speakers and Moderators:
| Presenter | Title | Date | Time | Session Type |
| Angela Hewlett, MD | RESPTC Support and Response | 10/20/2025 | 10:30 AM – 11:45 AM | Symposium |
| Nicolas Cortes-Penfield, MD | The Role of Rifampin in Hardware Infections | 10/22/2025 | 3:15 PM – 3:40 PM | Symposium |
| Mark Rupp, MD | Prevention of Blood Culture Contamination: Technique or Technology? | 10/20/2025 | 3:40 PM – 4:05 PM | Symposium |
| Sara H Bares, MD | Implementing Long-Acting ART | 10/20/2025 | 10:55 AM – 11:20 AM | Symposium |
| Sara H Bares, MD | Voices in Infectious Diseases | 10/21/2025 | 10:30 AM – 10:55 AM | Narrative Session |
| Jennifer M. Davis, MD | Challenging HIV Clinical Cases | 10/22/2025 | 1:45 PM – 3:00 PM | Interactive Session [Moderator] |
| Josh Havens, PharmD | Updates on Implementation Strategies for HIV Prevention | 10/21/2025 | 10:55am-11:20am | State-of the ART |
| Josh Havens, PharmD | Proven LAI Implementation Strategies in HIV Prevention and Treatment | 10/20/2025 | 7:00pm-9:00pm | Affiliated Event |
| Trevor Van Schooneveld, MD | Careers in Antimicrobial Stewardship | 10/19/2025 | 9:50am-11:15am | Fellows Workshop |
| Trevor Van Schooneveld, MD | Pneumonia PCR Panels Lead to a De-Escalation of Antibiotic Use-Con | 10/21/2025 | 2:15pm-3:30pm | Pro-Con Debate |
| Jasmine R. Marcelin, MD | Prioritizing Equity in Antimicrobial Stewardship Efforts (EASE): A Framework for Clinicians | 10/22/2025 | 10:50am-11:10am | Symposium |
| Jonathan Ryder, MD | Why You Need Diagnostic Stewardship | 10/22/2025 | 9:30am-9:55am | BugHub World Stage |
| Jasmine R. Marcelin, MD | The Next Frontier: Rapid AST to Optimize Care of Patients with Bloodstream Infections | 10/19/2025 | 10:00am-11:00am | Affiliated Event |
| Jasmine R. Marcelin, MD | Antimicrobial Prescribing Disparities and the Pursuit of Pharmacoequity | 10/18/2025 | 8:10 AM – 9:00 AM | Preconference Workshop |
| Andrea Zimmer, MD | Vincent T. Andriole ID Board Review Course | 10/18/2025 | 7:00am-4:30pm | Workshop [Course Director] |
| Andrea Zimmer, MD | IDBugCrawl – 31 Flavors of ID | 10/20/2025 | 1:00pm-2:00pm | |
| Andrea Zimmer, MD | Bridging the Gap Between General and Transplant Infectious Disease Practice | 10/20/2025 | 8:00 AM – 8:25 AM | BugHub [Moderator] |
| Andrea Zimmer, MD | Immunocompromised Host Community of Practice | 10/21/2025 | 5:00pm | Reception and Poster Walk |
| Angela Hewlett, MD | Lessons Learned in Biopreparedness and Biocontainment: Lassa Fever in the Midwest | 10/20/2025 | 10:30-11:45 | Symposium [Moderator] |
Oral Abstract Presenters
| Presenters | Title | Date | Time | UNMC ID Coauthors |
| Mackenzie R. Keintz, MD | Unlocking Knowledge: Designing an Infectious Diseases-themed Escape Room for Medical Student and Resident Education | 10/21/2025 | 3:15-4:30 (speaking slot 4:03-4:15) | Catherine Cichon, MD, Evangeline Green, DO, MPH, Jasmine R. Marcelin, MD, Benjamin K. Arbeiter, MD |
| Calvin Albrecht, MD [Fellow] | Case Presentation #3 – Fever and Constitutional Symptoms in a Young Returning Traveler | 10/20/2025 | 10:30 AM – 11:45 AM | |
| Jennifer M. Davis, MD | Insurance Changes are Common and Associated with Delayed Cabotegravir Plus Rilpivirine Injections | 10/22/2025 | 10:30am – 11:45am | O’Neill J, Lyden E, Bares SH |
| Emily Dyer, MD [Fellow] | Who’s Being Missed? Baseline Evaluation of Colorectal Cancer Screening in a Ryan White Population | 10/20/2025 | 2:30-2:45pm | Regan N, Bares SH, Lyden E, Davis JM |
| Josh Havens, PharmD | Real-World Insights of the Financial Metrics of a Long-Acting CAB-RPV Program | 10/21/2025 | 2:45 – 2:57pm | O’Neill J, Kubat M, Davis JM, Fadul N, Lechner J, Bares SH, Sunagawa S |
| Nicole Kusnik, MD [Fellow] | Intended and Unintended Conswquences of a Blood Culture Bottle Shortage: Changes in Antibiotic Prescribing, Contamination Rates, and Sepsis Measures at a Large Academic Institution | 10/21/2025 | 3:15-4:30 | Dr. Teran, Dr. VanSchooneveld, and Dr. Ryder |
| Albert Wu, MD [Fellow] | Blastomycosis in Vermont and New Hampshire | 10/21/2025 | 1:45 – 3:00pm |
Poster Presenters
| Presenter | Title | Poster number | Date | Time | UNMC ID Coauthors |
| Evangeline Green, DO, MPH [Resident] | Oral Antibiotic Stepdown Therapy for Uncomplicated Enterococcus Blood Stream Infections: A Retrospective Cohort Study | P-882 | 10/21/2025 | 12:15-1:30 | Cristina Torres, MD, Elizabeth Lyden, MS, Jasmine R Marcelin, MD, Mackenzie R Keintz, MD |
| Scott J. Bergman, Pharm D | Evaluation of oral antibiotic prescribing for uncomplicated Gram-Negative bloodstream infections following implementation of institutional guidance at an academic medical center | P-28 | 10/20/2025 | 12:15-1:30 | Joshua Lechner, PharmD, Mackenzie R. Keintz, MD, Jasmine R. Marcelin, MD, Molly M. Miller, PharmD, Elizabeth Lyden, MS, Jihyun Ma, MS, Trevor C. Van Schooneveld, MD, |
| Calvin Albrecht, MD [Fellow] | Is Respiratory Gram Stain Useful in the Era of Rapid, Highly Sensitive Molecular Pneumonia Panels? | P-612 | 10/20/2025 | 12:15 PM – 1:30 PM | Matthew Anderson, Elizabeth Lyden, Jonathan Ryder, and Trevor Van Schooneveld |
| Angela Hewlett, MD | Biopreparedness and Biocontainment Education in U.S. ID Fellowships | 10/22/2025 | 12:15 PM – 1:30 PM | Cristina Torres, David Brett-Major, James Lawler, Dan Cybulski, Gavin Harris, Elizabeth Schnaubelt | |
| Anna Kilzer [Student] | Biopreparedness Education in US Medical Schools | 10/22/2025 | 12:15 PM – 1:30 PM | James Lawler, Angela Hewlett | |
| Jillian Mack, PharmD [ID Pharmacy Resident] | A Stewardship Focused Evaluation of Patients Treated with Ceftriaxone for Infections due to Penicillin Susceptible Streptococcus spp. in Outpatient Parenteral Antimicrobial Therapy | 10/22/2025 | 12:15 PM – 1:30 PM | Nicolás Cortés-Penfield, Richard Hankins, Molly Miller, Elizabeth Lyden, Melissa LeMaster, Sara Azimi, Scott Bergman, Trevor C. Van Schooneveld, Mark E. Rupp, Bryan Alexander | |
| Shawnalyn Sunagawa, PharmD | Clinically Significant Adverse Event Rates for Daptomycin Outpatient Parenteral Antimicrobial Therapy | 10/22/2025 | 12:15 PM – 1:30 PM | Richard Hankins, Nicolas Cortes-Penfield, Bryan Alexander, Melissa LeMaster, Molly Miller | |
| Nicolas Cortes-Penfield, MD | Complete device extraction optimizes cure in deep brain stimulator & responsive neurostimulator device infections | P-126 | 10/20/2025 | 12:15-1:30pm | |
| Josh Havens, PharmD | Scalability Metrics and Effort Requirements for a Long-Acting CAB/RPV Program | 1871 | 10/22/2025 | 12:15-1:30pm | Kubat M, Davis JM, Fadul N, Havens J, Bares SH, Sunagawa S, Havens JP |
| Duncan Works [Student] | Outcomes of a Learning Needs Assessment Survey in the Development of the Extension for Community Health Outcomes Model for HIV Training in Midwestern Non-Metropolitan Areas | 1891 | 10/22/2025 | 12:15-1:30pm | Cramer D, Essam Nkodo EN, Lyden E, Zhan Y, Furl R, Fadul N, Davis JM |
| Vanessa Lo [Student] | Assessing Doxycycline Post-Exposure Prophylaxis (doxy PEP) Engagement in Care at a Midwestern HIV/PrEP Clinic | 333 | 10/20/2025 | 12:15-1:30pm | Havens JP, Bares SH, Davis JM, Scarsi KK, Sunagawa S |
| Jessica Witt, PharmD [MATEC Clinical Scholar] | Assessing HIV Pre-Exposure Prophylaxis Coverage at a Midwest Federally Qualified Health Center (FQHC) | 743 | 10/20/2025 | 12:15-1:30pm | Havens JP, Bares SH, Downes JM, Davis JM, Dworak A, Carter M, Sunagawa SW |
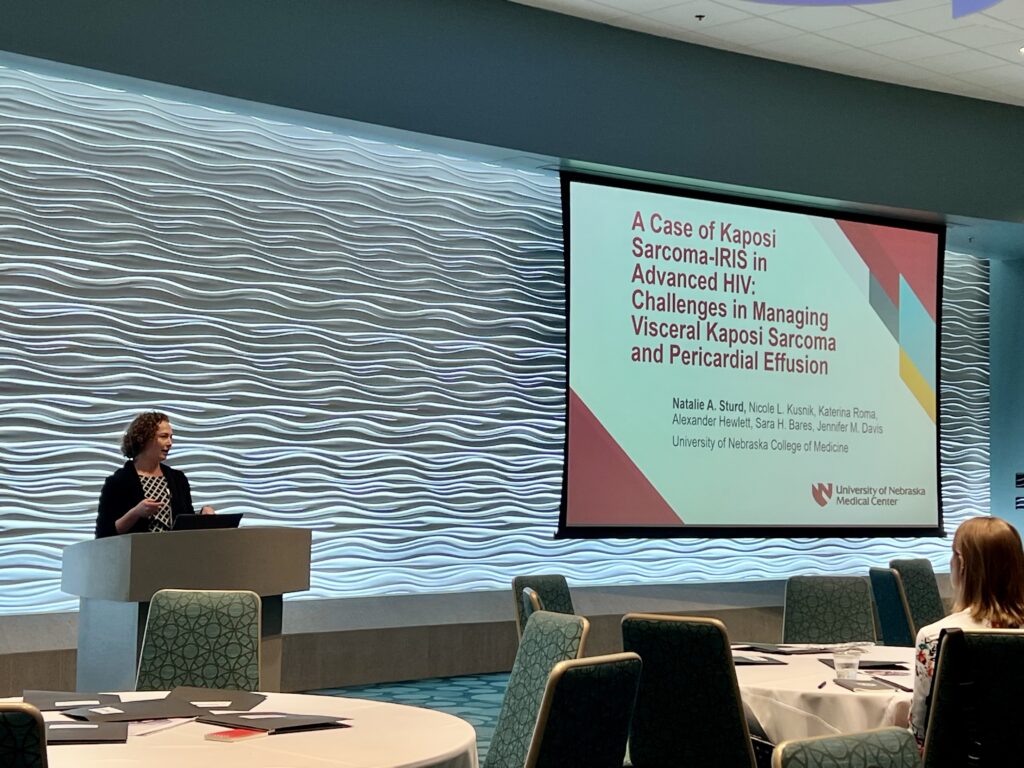
| Nicole Kusnik, MD [Fellow] | A young man with advanced HIV who presented with shortness of breath and splenomegaly | 2214 | 10/22/2025 | 12:15-1:30pm | Sturd NA, Roma K, Hewlett A, Bares SH, Davis JM |
| Emmanuel Nazaire Essam Nkodo, MD, MPH | Beyond Distance: Social Barriers Influence Long-acting Antiretrovirals Location Preference Among People with HIV in Rural Areas | P-2061 | 10/22/2025 | 12:15 PM – 1:30 PM | Renae Furl, Elizabeth Lyden, Daniel Cramer, Jennifer O’Neill, Maureen Kubat, Heather Saarela, Titilola Labisi, Nada Fadul. |
| Priscila Rodrigues Armijo, MD | Outcomes of a Statewide Educational Intervention Focused on Reducing COVID-19 Health Disparities Through a Quality Improvement Approach. | Salman Ashraf, Adati Tarfa, Elizabeth R. Lyden, Jasmine Marcelin, Jonathan H. Ryder, Jeff Wetherhold, Mahelet Kebede, Subhadra Mandadi, Precious S. Davis, Shirley Delair, Kelly Cawcutt, Andrea D. Jones, Mahliqha Qasimyar, Gail M. Etherton, Erica Stohs, Nada Fadul | |||
| Trevor Van Schooneveld, MD | Effect of Clinical Guideline Implementation on Use of Plasma Microbial Cell-free DNA Sequencing Testing at an Academic Medical Center | P-837 | 10/21/2025 | 11:15am-12:30pm | Tess Karre, Jonathan Ryder |
| Mackenzie Starlin [Student] | Measuring the Clinical Impact of a Novel Infectious Disease Step-Down Service | P-1874 | Makenzie Starlin, Rick Starlin, Bryan Alexander, Molly Miller, Kaeli Samson, Trevor C. Van Schooneveld | ||
| Samantha Moreno [Student] | Early Exposure to Infectious Diseases Specialty Among Undergraduate Students with Interests in Healthcare Careers | 10/22/2025 | 12:15pm-1:30pm | Jasmine R Marcelin | |
| Juan Teran, MD | Understanding Infection Control Needs in Nebraska Schools: Insights from School Health Staff | P-1888 | 10/22/2025 | 12:15 – 1:30 PM | Chris Cashatt, Mounica Soma, Salman Ashraf, Kate Tyner, Andrea Riley, Alice Sato, Robin Williams |
| Juan Teran, MD | Patterns and Prevalence of Carbapenemase-Producing Organisms Identified in Nebraska Healthcare Facilities Following Whole Genome Sequencing (2019-2024) | P-1069 | 10/21/2025 | 12:15 – 1:30 PM | Kathryn Burbach, Ishrat Kamal-Ahmed, Salman Ashraf, Amy Roden, Peter Iwen, Michael Wiley |
| David Warren, MD | Impact of Chlorhexidine Gluconate (CHG) Bathing on Bloodstream Infection Rates in Hematology-Oncology and Hematopoietic Stem Cell Transplant (HO/HSCT) Units | 10/21/2025 |
Award Winners
We are also thrilled to announce that all three of our senior fellows and two of our ID pharmacists are recipients of IDWeek Abstract Awards! Congratulations on your hard work!



IDWeek is more than a conference—it’s a convergence of minds dedicated to advancing infectious diseases research, education, and patient care. UNMC’s strong presence reflects our division’s commitment to leadership in the field and its ongoing efforts to address the most pressing challenges in ID.
Whether you’re attending in person in Atlanta or joining virtually, be sure to support our UNMC ID colleagues and celebrate their contributions to the field. See you there!
















Recent Comments