We are excited to welcome Jeremy Tigh PharmD as a new PGY-2 in our ID Pharmacy Residency Program! He’s the third ID Pharmacy resident we have had and a fantastic addition to our team! Read on to learn a little more about him…
Tell us about the position you recently started
I am beginning my second year as a pharmacist resident, specializing in infectious diseases. Over this year I will have comprehensive clinical training in antimicrobial stewardship and infectious diseases pharmacy practice. I will round with the inpatient infectious diseases consult services, participate in antimicrobial stewardship, OPAT, and community outreach stewardship programs, and practice in the HIV clinic longitudinally.
Tell us about your background
I grew up in Minden, Nevada, a small town tucked up next to the Sierra Nevada Mountains and Lake Tahoe. I completed my undergraduate studies at Utah State University and majored in cell and molecular biology. After graduating, I worked for a local biotechnology company as a research and development laboratory technician focused on mammalian cell culture. During that time I became increasingly interested in the world of pharmacy and subsequently attended pharmacy school at the University of Utah. After graduating, I left the mountains for the plains and completed my PGY1 pharmacy residency at Nebraska Medicine.
Why did you choose to come work at UNMC
When it came to applying to pharmacy residency programs, I wanted a program that offered a robust PGY1 experience but also had a well-established infectious diseases/antimicrobial stewardship program. I had heard good things about UNMC from my faculty mentor who trained there, and she encouraged me to apply. After interviewing, I was drawn by the family-friendly atmosphere of Omaha and the endless opportunities within UNMC. I was fortunate enough to match here for my PGY1, where I was able to get first-hand exposure to the serious medicine and extraordinary care that Nebraska Medicine provides, especially in antimicrobial stewardship and infectious diseases. I’m grateful to be able to stay for another year, where I will get to train under experts in the field and be a part of one of the best programs in the country!
What makes you excited about working in ID
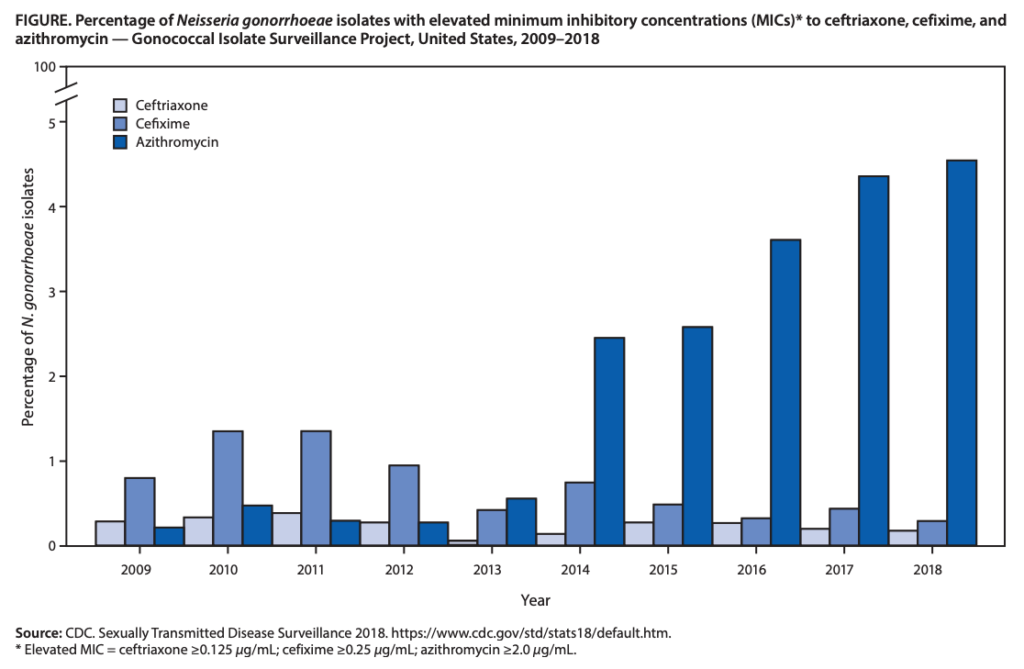
I think that it is important to choose a specialty that interests you the most; one that you will not mind spending a lifetime reading about, memorizing information, and teaching. For me, that is infectious diseases! I love the interplay between microbiology, antimicrobial resistance, stewardship, and drug PK/PD. I get the opportunity to learn about patients, but also microorganisms and therapeutics. This appeals to me as a lifelong learner and challenges my natural curiosity as things are constantly evolving. I am motivated by the belief that there are significant therapeutic challenges in this area for patients, physicians, and other healthcare professionals, and that as a pharmacist, I will have a leading role in helping to solve them.
Tell us something about yourself that is unrelated to medicine
My wife and I have a four-year-old daughter and are expecting a baby boy this Fall! We also have two black cats named Lottie and Darcy, and a bearded dragon named Poptart.







Recent Comments