Measles is one of the most contagious infections and is acute respiratory viral infection currently causing an outbreak of infection through the United States. Measles was first described hundreds of years ago and became a reportable infection in the US in 1912. In 1963, the first vaccine for measles became available. Efforts focused on measles elimination starting in the late 1970’s and with increased vaccination rates, measles was declared eliminated in the US in 2000.
Illustrator: Alissa Eckert CDC/ Allison M. Maiuri, MPH, CHES
What’s the Big Deal?
As of May 17, 880 cases of measles have been confirmed in the US this year making this outbreak the largest in the US since 1994 (before elimination in 2000). The number of cases continues to rise and thus far, 24 states have reported at least 1 measles case. Thus far, Nebraska has had a confirmed case of measles, but certainly the risk remains present as neighboring states (including Iowa, Missouri, and Colorado) have reported measles.
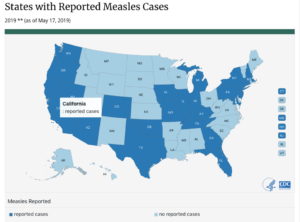
https://www.cdc.gov/measles/cases-outbreaks.html
How did this happen?
The risk for spread of measles has existed despite US elimination as the infection can be secondary to imported cases from travel as globally, measles has not been eliminated. The risk of transition has been augmented with the increased number of parents opting to not vaccinate their children against measles (via the MMR vaccine; see more about the vaccine below), thus there are increased opportunities for nonimmune, unvaccinated persons to develop infection and subsequently spread measles. Up to 90% of nonimmune people with a close exposure to measles will develop the infection. Measles is very contagious and can spread through the air. People with measles can infect others even before the classic rash appears, increasing the possibility of spreading the infection unknowingly.
Clinical Presentation
After exposure to the measles virus, symptoms usually appear between 7 and 14 days, however, may still develop for up to 21 days.
Measles usually presents with high fever, malaise and the 3 C’s: cough, coryza (runny nose) and conjunctivitis (red and watering eyes). Two to three days after symptoms arise, tiny white spots may appear inside the mouth, known as Koplick spots. Three to five days after onset, the classic rash of measles breaks out starting as flat red spots starting on the head and face and extending downward over the rest of the body. These spots may connect to create large patches of red. When the rash appears, it may high temperatures ( even over 105 degrees F) may arise. (images can be found here: https://www.cdc.gov/measles/about/photos.html) Measles is contagious for 4 days before the onset of the rash to 4 days after it develops.
Complications: Measles can be very serious, resulting in hospitalization in approximately 1 in 4 patients and even death (in 1-2 of every 1000 infected children). Additional complications include: bronchitis and/or pneumonia, otitis media, diarrhea and acute encephalitis. The acute encephalitis can cause permanent brain damage at the time of infection, and those with measles can also suffer from subacute sclerosing panencephalitis (SSPE) 7 to 10 years after their initial infection. SSPE a degenerative disease of the central nervous system that is fatal, but rare.
Diagnosis: The test of choice is a PCR test before day 9, after that , serology testing is more effective. This remains a reportable disease, so testing will need to go through local public health laboratories and departments.
Treatment: There is no specific treatment to cure measles. For those who are not immune, or have weakened immune systems, vaccines and infusions of immunoglobulins may be used to prevent measles, or at least decrease the severity of infection.
Prevention Spread of Disease:
Transmission: Measles is one of the most contagious of all infectious diseases; up to 9 out of 10 susceptible persons with close contact to a measles patient will develop measles. The virus is transmitted by airborne spread, therefore in clinics or hospitals, if you present with symptoms (or care a healthcare worker caring for them) N95 masks should be used. If not available, a surgical mask should be used. Measles virus can remain in the air for up to two hours after an infected person leaves.
Post-exposure Prophylaxis
If you have been exposed to measles, if you cannot show you have evidence of immunity against measles via documentation of vaccine or age. If these are no readily available, post-exposure prophylaxis with the vaccine (within 72 hours of exposure for healthy individuals) or immune globulin infusions (within 6 days of exposure). Of note, both of these should not be given for a single exposure event.
Outside of the healthcare setting, after receiving the MMR vaccine for a known exposure, people can return to school or work. For healthcare workers without evidence of immunity, from 5 to 21 days post-exposure they should be excluded from work.
Vaccine Specifics:
Measles vaccine is usually combined with mumps and rubella (MMR), or with mumps, rubella and varicella (MMRV).
Everyone should be assessed for immunity via documentation MMR/MMRV vaccinations or if adults are born during or after 1957 (before this assumed to have immunity UNLESS they are a healthcare worker, then immunity should be confirmed or vaccination considered).
Children – should have 2 doses of vaccine. 1 between age 12-15 months and 1 between 4-6 years.
Adults born during or after 1957 ( or currently under age 63): should have at least one documented dose of vaccine with the exception of the following, who should have a 2nd dose:
- Postsecondary educational students
- International travelers
- Healthcare personnel
- Persons with HIV and a CD4 count ≥ 200 cells/μl for at least 6 months
- Household or close personal contacts of immunocompromised persons with no evidence of immunity.
Stay Informed:
https://www.cdc.gov/features/measles/
https://www.cdc.gov/measles/resources/parents-caregivers.html.
https://www.cdc.gov/vaccines/parents/parent-questions.html.
https://www.cdc.gov/vaccines/parents/diseases/child/measles.html.
https://www.cdc.gov/measles/index.html
https://www.who.int/immunization/diseases/measles/en/
https://www.paho.org/hq/index.php?option=com_topics&view=article&id=255&Itemid=40899&lang=en
Latest updates for Nebraska can be found here: http://dhhs.ne.gov/Pages/Health-Alert-Network.aspx
