Research Digest is a periodic installment that recognizes the world-class clinical research performed right here at UNMC ID. Today, we review three articles covering the efforts to utilize research to improve the way we practice medicine, from optimizing the work environment to making it easier to find the most up-to-date recommendations. As always, check out the linked full articles for more details.

The first article, co-authored by our own Dr. Angela Hewitt and Dr. James Lawler of the UNMC Global Center for Health Security, discussed the impact of heat strain and dehydration on healthcare workers who must wear personal protective equipment (PPE) as they care for patients with high-consequence infectious diseases. The authors conducted a literature review of 30 articles that analyzed the effect of PPE on providers and concluded that there is much benefit to be gained from the development of cooler and more comfortable PPE materials. Such developments could slow the rate of dehydration and reduce heat strain on front-line workers caring for those with serious infectious diseases. Read the full details here.
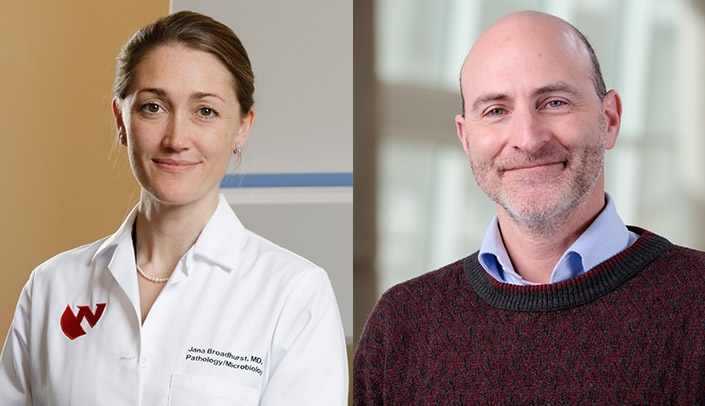
The next article, authored by many UNMC faculty members, including Dr. Jana Broadhurst and Dr. David Brett-Major, explored the use of a new generation of cost-effective biocontainment units called ISTARI (Isolation System for Treatment and Agile Response for High-Risk Infections). Designed to provide negative-pressure rooms in low-resource areas and decrease PPE use in the setting of highly infectious diseases, each unit is designed to perform ~20 air exchanges/hour with HEPA filters and multiple access points for providers to perform patient care without entering the unit, decreasing overall PPE usage. While some limitations were noted, providers rated their ability to perform their job roughly equivalent to the standard care scenario. 100% of teams met critical actions for patient management, including intubation, cardioversion, and CPR! This establishes the ISTARI unit as a cost-effective isolation unit, maximizing provider safety in managing patients with highly infectious diseases, particularly in low-resource settings. Read the full story here.

The last article, co-authored by Dr. Kelly Cawcutt, outlines ways to improve the dissemination of new medical information, such as that which changes rapidly (i.e., COVID-19 best practices). The Structured Team-based Optimal Patient-Centered Care for Virus COVID-19 ICU Collaborative is a 6-month project that trains volunteer interprofessional teams on the Checklist for Early Recognition and Treatment of Acute Illness and Injury approach, a structured and systematic method for delivering evidence-based critical care. The included weekly 1-hour videoconference sessions on high-impact topics, monthly quality improvement coaching sessions, and extensive additional resources for asynchronous learning. The program was well-received by participants and led to the initiation of several quality improvement projects. Read the paper here.