As our institution, state, country, and the world grapple with the impacts of SARS-CoV-2, causing COVID-19, there are lots of ongoing discussions about coronaviruses. Dr. Raquel Lamarche is a PGY1 Internal Medicine/Pediatrics resident at UNMC, who will be sharing her thoughts and information she learns about COVID-19. You can follow Dr. Lamarche on Twitter @LamarcheRaquel. This week Dr. Lamarche discusses “The Reopening”.
“The Reopening”
At this point, (at least) the more privileged members of society are aware of the benefits of social distancing. Now we are experiencing its negative offshoots, to mention a few: schools are closed, the economy is crumbling, and as Dr. Julia Marcus Ph.D. said, “Quarantine Fatigue is Real.” In her article, Dr. Marcus discusses sustainable risk reduction and how shaming risky behaviors drives them underground. My brother, a psychologist in the Dominican Republic interested in addiction and minorities, was often criticized for providing free needles and syringes to IV drug users to decrease their risk of bloodborne infectious diseases. Preventing all bad from happening, e.g., preventing people from physically socializing (ever), was never a realistic expectation. Harm reduction (secondary and tertiary prevention) are as valuable as primary and primordial prevention (trying to prevent the harm in the first place), in the sense that it meets our public health aspirations with public reality.
Since late April, the first states began to lift the restrictions placed to control the coronavirus pandemic. The lifting of restrictions has been controversial. Dr. Fauci testified before the Congress that reopening too soon could lead to unnecessary suffering and deaths. Here in Nebraska, we never had a formal “shelter in place” executive order shutting down the state; instead, there were a series of strict Directed Health Measures which are now gradually being relaxed. Following the news lately, there are many opinions on what “reopening the economy” means.
(See which states are re-opening and which states are still shut down)

What about herd immunity? In the US, the seroprevalence of SARS-CoV-2 is unknown, with obstacles including limited testing availability, and limited reliability of antibody tests. Scientists are still investigating how antibodies elicited by SARS CoV-2 may effectively neutralize the virus and for how long. The basic reproductive number, or R0, for SARS- CoV-2 is estimated to be 2, not as high as (real) airborne viruses such as varicella and measles (4, and 13, respectively). This means: one person with COVID-19 can spread the virus to 2 other persons (or more if they are singing in a choir). Herd immunity is the indirect protection provided to individuals in a community when most of the population is immune to that disease. Based on the R0 of SARS-CoV-2, it is thought that 60-70% of the population needs to have contracted SARS CoV-2 in order to start seeing the benefits of herd immunity, and it is unlikely that we have achieved this yet. We have achieved herd immunity to other infections like measles and chickenpox due to vaccine uptake in the community.
Vaccine? When? Vaccines can be hard to develop. There are over 60 vaccine trials right now. The hope is that with so many trials going, we will have at least one vaccine at some point, maybe 18 months from now, we are talking about 2021 perhaps. Moderna found that its experimental SARS CoV-2 vaccine was safe and provoked a strong immune response in 8 healthy volunteers.
How should we approach the re-opening? Due to a lack of widespread testing, the initial “containment” attempt to limit the spread of this virus is long gone as a feasible idea (adios). The virus is close to all of us. The conversation we are having right now is about harm mitigation. To re-open as safely as possible, certain conditions need to be met:
- The rates of new cases should be low and remain low for at least two weeks.
- There should be capacity to test anyone who has COVID-19 symptoms
- Hospitals should be able to treat all cases.
Based on the above conditions, many states seem to be re-opening prematurely. But now that things are opening up, how can we stay safe?
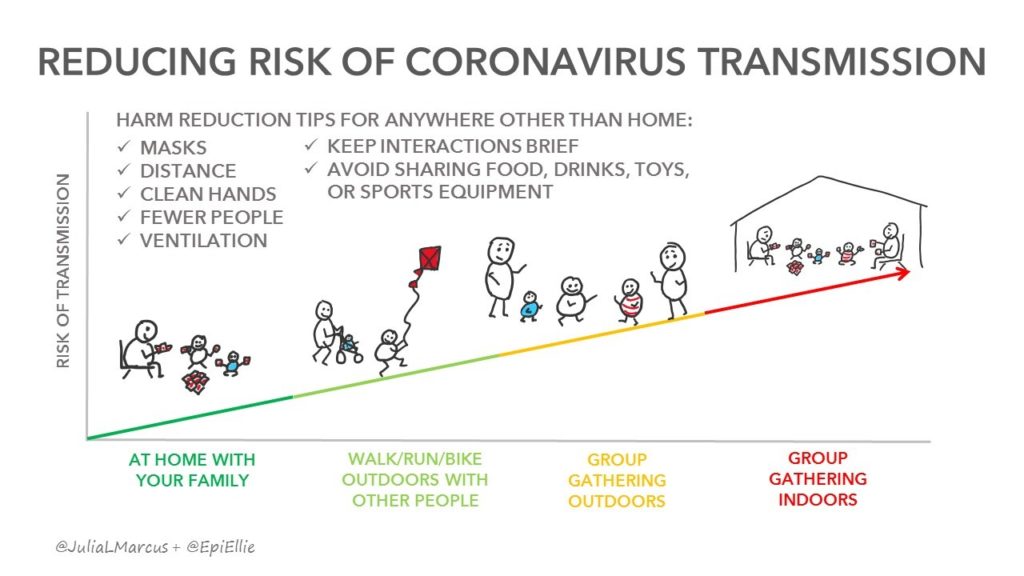
1. (Sustainable) social distancing. Continue to stay 3-6 feet or more away from each other. Dr. Marcus talks about sustainable risk reduction strategies in her article, with some outdoor activities (such as walking, running, and cycling) posing less risk than indoor gatherings.
2. Hand Hygiene. We must wash hands as often as possible, especially every time we go into a new environment. Linking handwashing to mindfulness (e.g., acknowledging four tactile sensations while handwashing) has helped me reframe the experience. Also, clean surfaces at least once per day at the very minimum.
3. Perfect surveillance and contact tracing. The process should involve quarantining positive cases, followed by tracing then testing all of their contacts. In order to limit the spread of the virus, we must have the ability to test anyone who might have SARS-CoV-2. Dr. Atul Gawande, in his NewYorker article, described daily screening of all employees, patients, and visitors for symptoms of COVID-19 upon entry to any building in his healthcare system. UNMC has recently implemented a universal screening policy for all admitted patients.
4. Wear a mask! If worn appropriately, masks can help keep individuals from spreading their own droplets to others. The critical point is that these kinds of masks don’t create a perfect seal and are not meant to protect yourself: they are meant to protect those around you. If worn by everyone, we protect each other. N95 respirators block most airborne particles from being inhaled, therefore are designed to protect the wearer too. Throughout the pandemic there has been an N95 supply-demand mismatch. As ways to circumvent this problem, there have been great innovations that can help us safely reuse N95s, such as:
• Ultraviolet germicidal irradiation by UNMC
• Hydrogen peroxide decontamination system by Battelle
How do we re-open the economy and our physical social lives while still keeping each other healthy? What is going to save us, a vaccine, herd immunity, or a new treatment? I know that I did NOT provide you with perfect answers. Viruses are sometimes too smart for drugs. We continue to lack the capacity for widespread testing and contact tracing. We are far from being immune. A vaccine is many months away.
More powerful than putting our energy on hopes for a miracle, is a strong performance at applying what we already know: physical distancing, hygiene, screening, staying at home if we are ill, and wearing a mask (correctly).
Stay safe everyone!

Very informative article! Sources of accurate information are really needed and appreciated these days. Thanks for posting!!
Thanks for such an easy to read And understand piece that I will share with some confused folks.Mask wearing is now getting a lot of misleading info. Saw video in which a young woman said wearIng a mask for 24 hours was so bad. So invalid examples are being paired with valid health info and some folks get confused.