
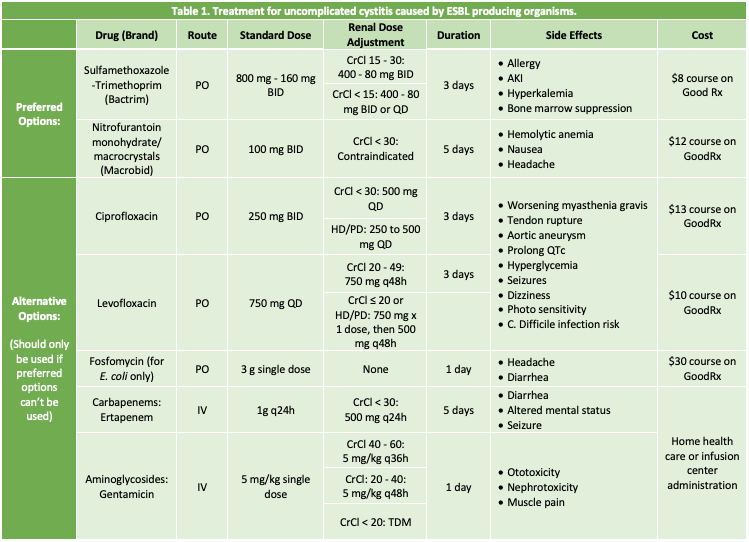
Part 1 of this #PharmToExamTable post explores treatment options for uncomplicated ESBL UTIs and was authored by Anna Rehberg, 2024 UNMC College of Pharmacy PharmD Candidate
(Content reviewed by: Jenna Preusker, PharmD, BCPS, BCIDP, Scott Bergman, PharmD, BCIDP, and Nicholson Perkins, PharmD)
Fast Facts about ESBL UTI treatment:
- People who have more healthcare exposure are more likely to get ESBL infections, but it can also be community-acquired.
- ESBL-producing organisms cannot be treated with oral beta-lactam antibiotics.
- Guidelines recommend uncomplicated cystitis caused by an ESBL-producing organism be treated with oral SMX-TMP or nitrofurantoin if they are susceptible.
- Guidelines recommend ESBL cUTIs and pyelonephritis be treated with oral SMX-TMP, fluoroquinolones, or IV carbapenems.
Introduction to ESBLs
ESBLs, or Extended Spectrum Beta Lactamases, are enzymes produced by Gram-negative bacteria that inactivate most penicillins, cephalosporins, and aztreonam while remaining susceptible to carbapenems in the absence of other resistance mechanisms.1 ESBLs do not inactivate non-beta lactam antibiotics such as levofloxacin, sulfamethoxazole-trimethoprim, fosfomycin, or gentamicin.1 However, organisms harboring ESBLs often contain additional mechanisms of resistance that could render these antibiotics ineffective. ESBLs can be found in any gram-negative organism but are most prevalent in Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca, and Proteus mirabilis.2 In the United States, the CTX-M enzyme is the most common type of ESBL present, accounting for approximately 80% of all ESBL infections nationally.1
ESBL infections occur most frequently in those with high healthcare exposure, particularly those requiring prolonged hospital stays, residents of skilled nursing homes, or residents of long-term acute care facilities, but they can also cause community-acquired infections in otherwise healthy people who have taken antibiotics before.3 Bacteria with ESBL enzymes can spread from person to person in healthcare settings or through contaminated food or water, just like other bacteria and microbes.3
IDSA guidelines do not provide recommended durations of therapy for ESBL infections, but expert clinicians advise the duration of therapy should not differ for infections caused by organisms with resistant phenotypes compared to infections caused by more susceptible phenotypes.1 Also, oral antibiotics can be an equally efficacious step-down therapy option when the patient meets the following criteria:1
- Hemodynamic stability
- Source control
- Susceptible to an appropriate, non-beta lactam, oral agent
- No concerns for insufficient intestinal absorption
What are preferred antibiotics for the treatment of uncomplicated cystitis caused by ESBL-producing organisms?
Nitrofurantoin and sulfamethoxazole–trimethoprim (SMX-TMP) are the preferred agents for the treatment of uncomplicated cystitis caused by ESBL-producing organisms.1 In an open-label non-inferiority study, five days of nitrofurantoin therapy was compared to three days of double-strength SMX-TMP for the treatment of uncomplicated cystitis.4 A total of 338 women, aged 18 – 45 years old, enrolled in this trial with the primary outcome of clinical cure at 30 days after therapy completion with secondary outcomes including cure rates at 5 to 9 days. Clinical cure was achieved in 79% of patients in the SMX-TMP group and 84% of patients in the nitrofurantoin group. Clinical and microbiological cure rates at first follow-up visit were equivalent between groups. Though this study did not exclusively evaluate ESBL cystitis, the authors concluded that a five-day course of nitrofurantoin is equivalent clinically and microbiologically to a three-day course of SMX-TMP and should be considered an effective fluoroquinolone-sparing alternative for the treatment of uncomplicated cystitis in women.4
Fluoroquinolones and carbapenems are also effective agents for treatment of uncomplicated cystitis caused by ESBL-producing organisms, but their use is discouraged in this disease state.1 Limiting the use of these agents reduces the risk of antibiotic adverse events and benefits patients in the future by preserving antimicrobial activity.1 In a randomized, single-blinded study done in 2005, a three-day course of amoxicillin-clavulanate and ciprofloxacin were compared for the treatment of uncomplicated cystitis.5 There was a total of 370 women enrolled, aged 18 – 45 years old, who were then randomized 1:1 into two groups. The results demonstrated the three-day regimen of amoxicillin-clavulanate was not as effective as ciprofloxacin for the treatment of acute uncomplicated cystitis, even in women infected with susceptible strains. Inferiority of amoxicillin-clavulanate was partially due to not fully eradicating E. coli from the vaginal area. This outcome can be explained by the increasing resistance to amoxicillin along with the length of time amoxicillin and clavulanate are in the serum (1.3 hours and 1 hour, respectively) compared to ciprofloxacin (4 hours). This study did not monitor side effects of fluoroquinolones, but general side effects for all medications mentioned can be seen in Table 1.5
Fosfomycin is also an option for the treatment of uncomplicated ESBL cystitis.1 However, infections caused by K. pneumoniae, Serratia marcescens, Enterobacter spp. and P. aeruginosa are resistant to fosfomycin due the presence of FosA genes.6 However, this gene is often absent in ESBL E. coli, so fosfomycin can be used as treatment in those cases.6 But in a study done comparing a five – day course of nitrofurantoin to a single dose of fosfomycin for uncomplicated cystitis clinical cure, fosfomycin only had a 58% cure rate compared to 70% in the nitrofurantoin group.7
To be continued next week…
References:
- Pranita D Tamma and others, Infectious Diseases Society of America 2023 Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections, Clinical Infectious Diseases, 2023;, ciad428, https://doi.org/10.1093/cid/ciad428
- Tamma PD, Smith TT, Adebayo A, et al. Prevalence of bla CTX-M Genes in Gram-Negative Bloodstream Isolates across 66 Hospitals in the United States. J Clin Microbiol 2021; 59(6).
- CDC. ESBL-producing Enterobacteriaceae. Centers for Disease Control and Prevention. Published 2019. https://www.cdc.gov/hai/organisms/ESBL.html
- Gupta K, Hooton TM, Roberts PL, Stamm WE. Short-course nitrofurantoin for the treatment of acute uncomplicated cystitis in women. Arch Intern Med. 2007;167(20):2207-2212. doi:10.1001/archinte.167.20.2207
- Hooton TM, Scholes D, Gupta K, Stapleton AE, Roberts PL, Stamm WE. Amoxicillin-clavulanate vs ciprofloxacin for the treatment of uncomplicated cystitis in women: a randomized trial. JAMA. 2005;293(8):949-955. doi:10.1001/jama.293.8.949
- Ito R, Mustapha MM, Tomich AD, et al. Widespread Fosfomycin Resistance in Gram-Negative Bacteria Attributable to the Chromosomal fosA Gene. mBio. 2017;8(4):e00749-17. Published 2017 Aug 29. doi:10.1128/mBio.00749-17
- Huttner A, Kowalczyk A, Turjeman A, et al. Effect of 5-Day Nitrofurantoin vs Single-Dose Fosfomycin on Clinical Resolution of Uncomplicated Lower Urinary Tract Infection in Women: A Randomized Clinical Trial. JAMA. 2018;319(17):1781–1789. doi:10.1001/jama.2018.3627