This post is part of a series on Antibiotic Awareness Week 2022, authored by Scott Bergman, PharmD, FCCP, FIDSA, BCIDP. Read on to learn more about influential antibiotic stewardship research published this year.
This year for Antibiotic Awareness Week, I want to revisit a few studies that I selected for my presentation at the recent IDWeek conference on Most Influential Papers in Antimicrobial Stewardship from the Past Year. These are by no means ranked in order of quality or impact, but rather tell a story of where we are in terms of research and practice this year.
The first paper I want to highlight is titled “Rural-urban differences in antibiotic prescribing for uncomplicated urinary tract infection” in Infection Control and Hospital Epidemiology.1 As we have become more aware of racial disparities in healthcare over the last few years, in Nebraska we have also thought about the difference in antimicrobial stewardship between our urban and rural areas of the state. This study included women 18-44 years old with uncomplicated UTIs from 2010-15 and classified them into groups based on their zip code as either rural or urban (metropolitan statistical areas > 50,000 population). Using insurance claims from the IBM Marketscan database, investigators evaluated whether prescriptions followed IDSA guidelines over this time period. Over 670,000 claims were reviewed to determine that almost half of prescriptions, 46.7%, were not for first-line antibiotics (table 1). To maintain that these were indeed uncomplicated, community-acquired UTIs, patients were excluded if they had been in the hospital within 90 days or received an antibiotic or had another infection with 30 days.
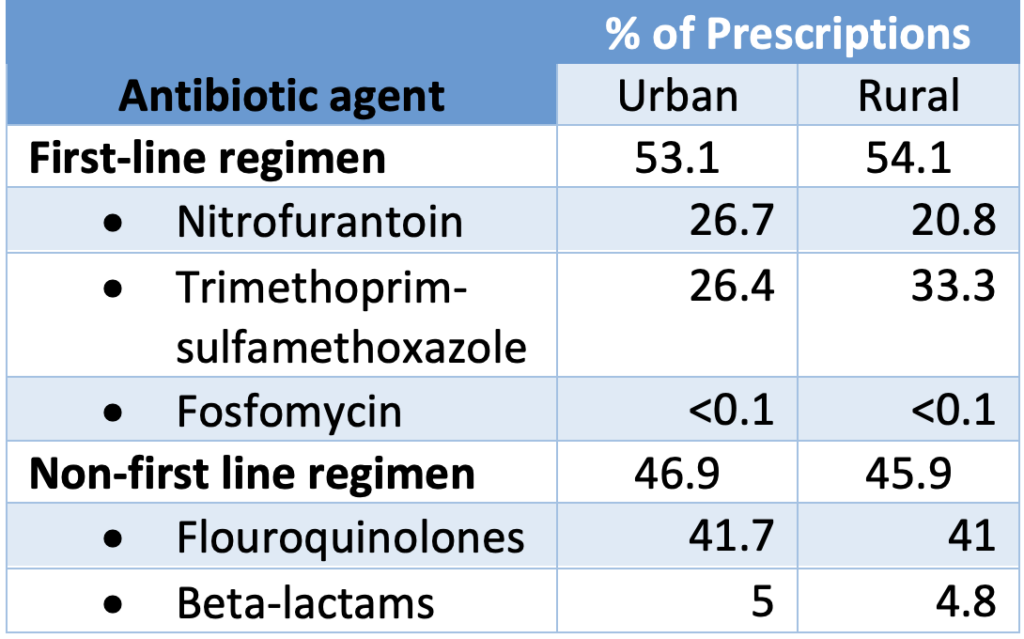
This rate of guideline-discordant prescribing was not significantly different between rural & urban geographical designations. It was in length of therapy where the difference became more apparent – with rural women receiving inappropriate durations 83.9% of the time compared to 74.9% of urban prescriptions (table 2). Regardless of the amount of that difference, neither of these statistics are encouraging. I left feeling that we that we have a lot of education to do for prescribers to feel comfortable giving the antibiotics recommended by guidelines for uncomplicated cystitis over the durations of therapy that are based on evidence.
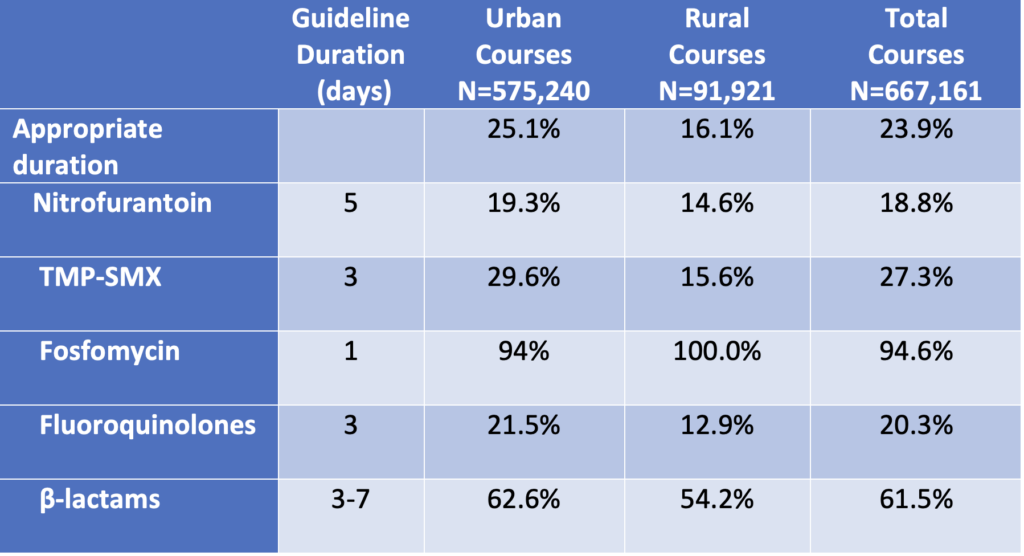
As you can probably guess, the durations prescribed were considered inappropriate for being longer than recommended 99% of the time. While a few days extra of an antibiotic may not seem like a big deal, the adverse effects associated with these courses can really add up, especially when we are talking about almost half a million inappropriate prescriptions in this study.
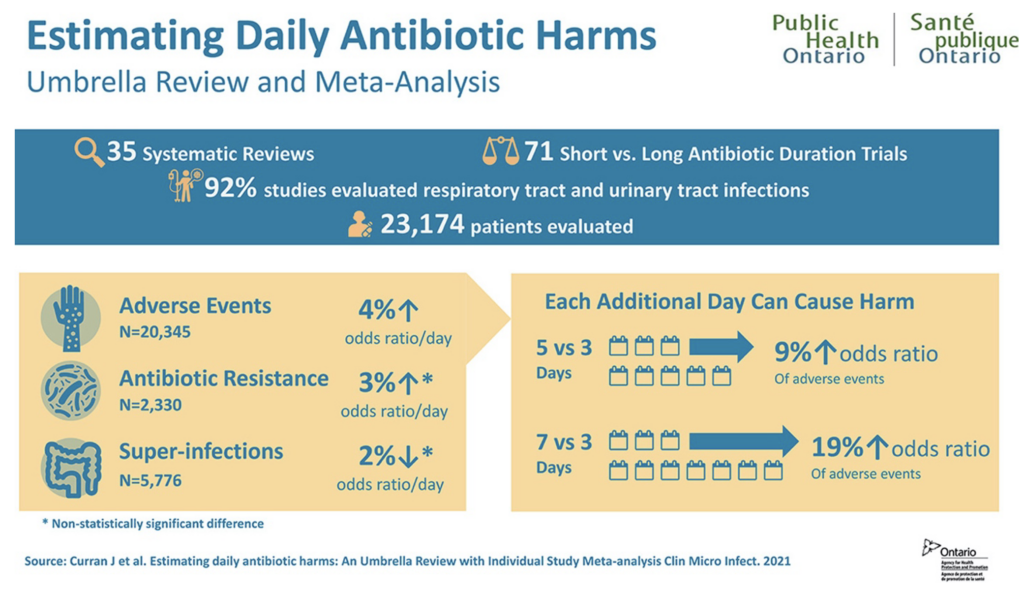
That brings me to the other important paper from the last year I want to cover, “Estimating daily antibiotic harms: an umbrella review with individual study meta-analysis”, published in Clinical Microbiology and Infection.2 This study conducted by Public Health Ontario was a meta-analysis of 71 randomized trials identified from 35 systematic reviews of shorter versus longer fixed durations of therapy ranging from 3 to 14 days. These studies were primarily for treatment of respiratory tract (n=36, 51%) and urinary tract infections (n=29, 41%). If you’ve ever read one of these many trials, you will know that the conclusion is almost always the same – shorter courses are equally effective to longer courses, but the adverse effects are greater in the long duration group. To quantify that, 23,174 patients were pooled in this analysis and 20,345 adverse effects were identified in 19.9% of patients these trials. Other documented harms associated with antibiotics included 5,776 superinfections in 4.8% of patients and 2330 cases of new resistance in 10.6% of patients. Overall, they concluded that each day of antibiotic therapy was associated with a 4% increased odds of having any adverse event. Furthermore, the risk of having a severe adverse event rose incrementally 9% for each subsequent day of therapy.
Combined, these two studies paint a fairly bleak picture for antimicrobial use in 2022, but there are bright spots as well. I don’t have time to elaborate, but I listed a few other studies below that I selected for my presentation on influential papers in antimicrobial stewardship which show benefit of education.

About the Author:
Scott Bergman, PharmD, FCCP, FIDSA, BCIDP
Pharmacy Coordinator, Antimicrobial Stewardship Program – Nebraska Medicine
Clinical Professor, University of Nebraska Medical Center – College of Pharmacy
References:
- Klatt ME, Schulz LT, Fleischman D Fox BC, Burke S, Grinder D, et al. Implementation of telehealth antimicrobial stewardship through a partnership of an academic medical center and community hospital. Am J Health-Syst Pharm. 2021 (Dec); 78: 2256-64
- Moehring RW, Yarrington ME, Warren BG, Lokhnygina Y, Atkinson E, Bankston A, et al. Evaluation of an Opt-Out Protocol for Antibiotic De-escalation in Patients with Suspected Sepsis: a multicenter randomized controlled trial. Clin Infect Dis. 2022 (Sep); Online ahead of print
- Molina J, Montero-Mateos E, Praena-Segovia J, Leon-Jimenez E, Natera C, Lopez-Cortes LE, et al. Seven-versus 14-day course of antibiotics for the treatment of bloodstream infections by Enterobacterales: a randomized, controlled trial. Clin Microbiol Infect. 2022 (Apr);28:550-557
- 1. Rural–urban differences in antibiotic prescribing for uncomplicated urinary tract infection. Infect Contr Hosp Epidem. 2021 (Dec); 42: 1437-44
- 2. Estimating daily antibiotic harms: an umbrella review with individual study meta-analysis. Clin Microbiol Infect. 2022 (Apr); 28: 479-90