The following content was originally written for the IDSA Journal Club by Dr. Kelly Cawcutt.
As we continue forward in a global pandemic of unprecedented proportions, prevention of continued transmission of SARS-CoV-2 remains critically important. There has been ongoing debate regarding the highest risk factors for transmission, including the risk of potential aerosolized virus versus primary droplet spread. Based on this debate, the appropriate levels of personal protective equipment for both frontline healthcare workers and the general public have also remained somewhat controversial.
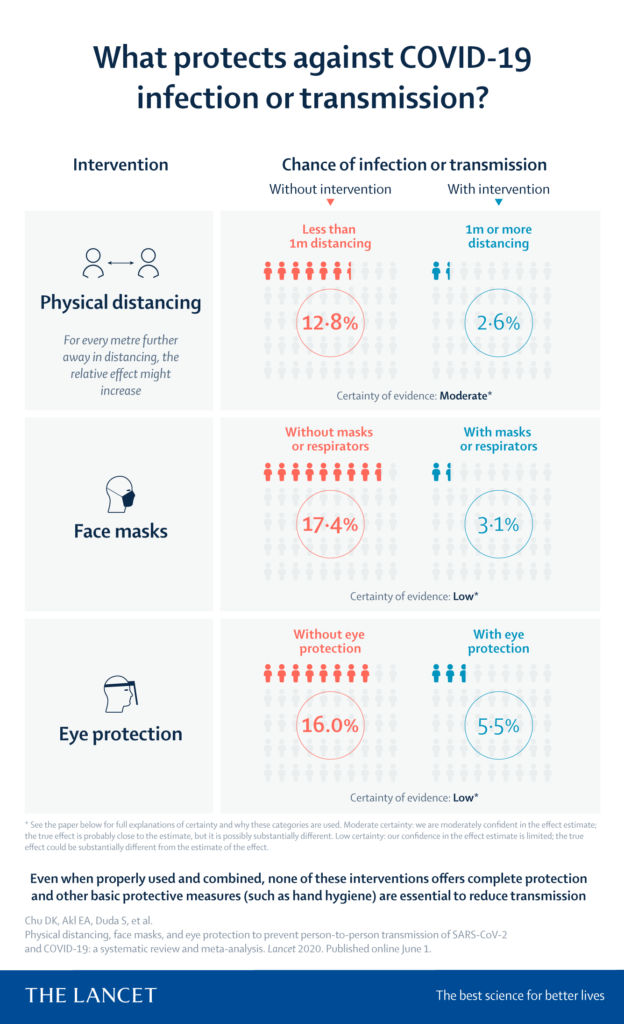
In an attempt to answer this question Chu et al recently published a systematic review and meta-analysis assessing physical distancing, face masks of varying types and eye protection within healthcare and non-healthcare settings, to determine if there is evidence for benefit to support ongoing recommendations of their use.
The systematic review included published research related to SARS, MERS and COVID-19. It is of note, that all studies were observational with no randomized controlled trials regarding these 3 infections. Results demonstrated that transmission of infection decreased with physical distancing of at least 1 m (adjusted OR 0.18; 95% CI 0.09-0.38) with a risk reduction of approximately 10% and increasing protection if the distance was extended to 2 m or greater. Additionally, the use of face masks in all settings was associated with decreased transmission of infection (adjusted OR 0.15, 95% CI 0.07-0.34) with a risk reduction of approximately 14%. There were some potential differences in mask type, with decreased transmission with respirators (N95) as compared to surgical or cloth masks. Finally, eye protection (including goggles, faceshields) also demonstrated decreased risk of transmissions with use (adjusted OR 0.22; 95% CI 0.12 -0.39) with the risk reduction of approximately 10%.
This study provides early evidence of the efficacy of continued PPE use to prevent transmission of COVID-19, both in the community and in the healthcare setting, including continued physical distancing, facemask use and eye protection. It should be noted that the impact as facemask and eye protection utilization is not adjusted for duration of time spent with an actively infected person nor the impact of physical distancing in the absence of the masks or eye protection. The variation of impact in different types of masks, including N95s, is difficult at best to interpret due to lack of randomized controlled trials, lack of information on aerosol generating procedures within studies, and potential variations both in mask quality, appropriate fit of masks, donning and doffing and hand hygiene.
Further research is clearly needed to optimize PPE utilization in the setting of existing shortages faced during this pandemic and for ongoing public health and infection control policy on healthcare based PPE recommendations.
Indeed, this is not over yet.