Content written by Dr. Mark Rupp.
Content written by Dr. Mark Rupp.
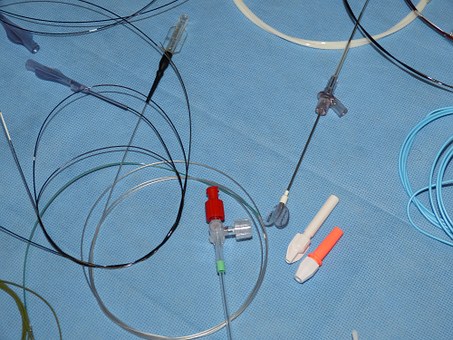
Impressive gains in the prevention of central line associated bloodstream infections (CLABSI) have been realized in recent years in US hospitals. However, with efforts to improve efficiency and decrease hospital length of stay, patients are increasingly being discharged to home health care to receive intravenous therapy. The rate of complications associated with vascular catheterization in the home care setting is largely undefined.
In a recent issue of the American Journal of Infection Control, authors Regina Nailon and Mark Rupp detail results from a surveillance system encompassing 10 home health agencies from 4 states over a 51 month period (Nailon RE, Rupp ME. Surveillance of Home Health Central Venous Catheter Care Outcomes: Challenges and Future Directions. American Journal of Infection Control 47:1382-1387, 2019). During a period of greater than 250,000 device days of observation, 913 catheter occlusions and 73 CLABSIs were noted. For adults, the occlusion rate was 5.87 events per 1000 catheter days and CLABSI occurred at a rate of 0.22 per 1000 catheter days. For pediatric age patients, the rates for occlusion and CLABSI per 1000 catheter days were 1.85 and 0.13, respectively. The data were reported to participating agencies on a quarterly basis with deidentified individual agency data compared to aggregate rates. Based on the quality reports, some agencies instituted quality improvement and noted substantial decreases in complication rates.
An unknown proportion of the millions of patients receiving home health care receive treatment through a vascular catheter. This study demonstrates that a small, but substantial, percentage of home healthcare patients experience serious adverse complications associated with intravascular catheters. Clearly, a comprehensive surveillance system is needed to monitor outcomes and improve practices in this sizable group of patients. The study also emphasizes the need for standardized education and care practices for patients and their families who provide a substantial portion of catheter care at home.
As James Harrington related: “Measurement is the first step that leads to control and eventually to improvement. If you can’t measure something, you can’t understand it. If you can’t understand it, you can’t control it. If you can’t control it, you can’t improve.”
Or, more succinctly… what gets measured, gets managed.