Targeted therapy and antimicrobial stewardship in patients with febrile neutropenia is difficult because in the vast majority of cases, an organism is not identified, and patients are known to be high risk for serious infections. Antibiotic de-escalation in patients with neutropenic fever varies, with European guidelines recommending 72hr de-escalation and North American guidelines recommending continuation of broad spectrum therapy until neutrophil engraftment.  Dr. Jasmine Marcelin presented a study in ID Journal Club recently that applied an antimicrobial stewardship intervention to this patient population.
Dr. Jasmine Marcelin presented a study in ID Journal Club recently that applied an antimicrobial stewardship intervention to this patient population.
Plain Language Summary: The study found that in patients whose blood counts had dropped due to chemotherapy that developed fevers with no identifiable cause, stopping antibiotics 5 days after fevers resolved did not lead to worse outcomes (as compared to continuing antibiotics until blood counts recovered).
Snyder et al; Early Antimicrobial De-escalation and Stewardship in Adult Hematopoietic Stem Cell Transplantation Recipients: Retrospective Review, Open Forum Infectious Diseases. https://doi.org/10.1093/ofid/ofx226
The authors of this study sought to provide a middle ground by assessing whether or not patients who were de-escalated after 5 days of therapy (but before engraftment) would have worse outcomes.
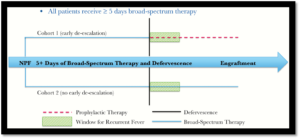 This was a single-center retrospective cohort study looking at allogeneic hematopoietic stem cell transplant (HSCT) patients with febrile neutropenia (who had defervesced and were clinically stable) who were de-escalated to neutropenic prophylaxis after 5 days (cohort 1) vs those who were continued on broad-spectrum therapy until engraftment (cohort 2). The study included 120 patients, with 46 in cohort 1 and 74 in cohort 2. The question: if patients are de-escalated after 5 days, are they more likely to have recurrent fever?
This was a single-center retrospective cohort study looking at allogeneic hematopoietic stem cell transplant (HSCT) patients with febrile neutropenia (who had defervesced and were clinically stable) who were de-escalated to neutropenic prophylaxis after 5 days (cohort 1) vs those who were continued on broad-spectrum therapy until engraftment (cohort 2). The study included 120 patients, with 46 in cohort 1 and 74 in cohort 2. The question: if patients are de-escalated after 5 days, are they more likely to have recurrent fever?
In the assessment of recurrent fever, early de-escalation was non-inferior to prolonged broad spectrum antibiotics (15% vs 19%, 90% CI -0.09 to 0.16, p 0.026). There was no difference in the occurrence or time to re-escalation/re-initiation of broad spectrum antibiotics. Additionally, there were no differences in down-stream effects such as length of stay, ICU admissions, Clostridium difficile infections or in-hospital mortality, and notably, no patients developed bloodstream infection after de-escalation, regardless of recurrent fever. Finally, in the early de-escalation group there were 0.6 days of gram-positive antimicrobial agents per patient compared to 1.7 days per patient in the group that received prolonged broad spectrum antibiotics (p=0.001).
While it certainly does NOT demonstrate that de-escalating after 5 days is better than continuing antibiotics until engraftment, there was no difference in clinical outcomes in patients who were de-escalated early compared with those continued on prolonged antibiotics, with added benefits of reduction of cost and antimicrobial utilization. The authors added that the results of this study have already led to changes in clinical practice at their institution.
The biggest limitation of this study was that it was retrospective: missing data is always a concern. How can we be sure that there were no uncontrolled variables that impacted duration of empiric antimicrobial therapy?
This article led to great discussion among the group, and fortunately our entire Oncology ID group was in attendance, including Dr. Alison Freifeld, first author of the 2011 IDSA Neutropenic Fever Guidelines and Director of our Oncology Infectious Disease Program here at UNMC ID. Dr. Freifeld commented that “we have been interested in early de-escalation for a while now“, and shared that their group have been even more aggressive than what is described here for early de-escalation. Dr. Andrea Zimmer added that while difficult to quantify, anecdotally there have not been high rates of post-de-escalation febrile illnesses even with aggressive de-escalation.
The Journal Club group also briefly discussed a related study, a recent randomized controlled trial, the “How Long Study” (Aguilar-Guisado, Manuela et al. The Lancet Haematology , Volume 4 , Issue 12 , e573 – e583). In this study, the authors found that in similar high-risk patients with hematologic malignancies or HSCT and febrile neutropenia, empiric therapy could be safely discontinued without neutropenic prophylaxis after 72hrs of being afebrile. Like the study by Synder et al., this RCT noted no difference in rate of recurrent fever, mortality, or other adverse events in the group with antibiotics discontinued compared with continuing empiric antibiotics until neutrophil engraftment.
While it remains to be seen whether early de-escalation or complete discontinuation is the best recommendation, both these studies demonstrate the value of antimicrobial stewardship in the immunocompromised population with febrile neutropenia. 
