Nebraska Medicine and Antimicrobial Stewardship in the Outpatient Setting
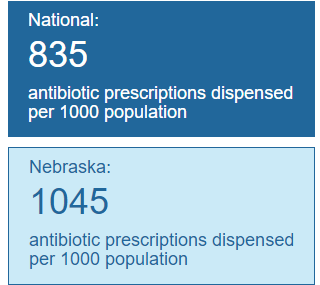
Antimicrobial stewardship is not only about inpatient prescribing. Recent studies measuring antibiotic use in ambulatory settings have estimated that antibiotics are prescribed inappropriately 30-77% of visits(1). Despite being one of the leaders in implementing antimicrobial stewardship in hospitals, Nebraska ranks 44th (out of 50 states and District of Columbia) in outpatient antibiotic prescriptions dispensed. The practice of inappropriate antibiotic prescribing is one of the factors that has led to world-wide spread of antibiotic resistant bacteria. Due to the ongoing issue of antibiotic resistance, in 2014 the president called for a 50% reduction in appropriate outpatient antibiotic use in his National Action Plan for Combating Antibiotic-Resistant Bacteria. In 2016, the Centers for Disease Control and Prevention (CDC) outlined the Core Elements of Outpatient Antibiotic Stewardship(2).
The CDC suggested that in order for an outpatient antimicrobial stewardship program to be successful, it needs leadership commitment within healthcare institutions, definitive action by implementation of policies to improve prescribing practices, accurate tracking of prescribing and individual reporting to prescribers, education of healthcare professionals and patients/families, and finally access to experts in antimicrobial stewardship. Put simply, the goal of these elements, when implemented, are to improve patient care by treating infections with antibiotics when needed, avoiding patient adverse effects (like drug toxicities or C. difficile infections) from unnecessary antibiotic treatment, and avoiding the development of antimicrobial resistance in the community.
Here at Nebraska Medicine we have several ongoing projects geared towards improving our antibiotic use in the outpatient setting. We have been working with hospital and ambulatory clinic leadership to improve vaccination protocols, particularly with an inpatient nurse-driven influenza protocol that identifies patients who need the flu vaccine and administers prior to discharging from the hospital. Alerts have also been developed in our electronic health record which prompt clinicians when vaccines are indicated. Additionally, we partnered with the Nebraska Health Network to develop evidence-based guidance documents for the treatment of sinusitis and C. difficile infections in the outpatient setting. Additional guidance documents focused on the inpatient setting are also applicable to outpatient encounters, such as Acute Exacerbations of Chronic Obstructive Pulmonary Disease (AECOPD), Urinary Tract Infections (UTI), Skin/Soft Tissue Infections (SSTIs), and Community Acquired Pneumonia (CAP).
Finally, we have partnered with the Nebraska Antimicrobial Stewardship Assessment and Promotion Program (ASAP) to create a large-scale antimicrobial stewardship education program for ambulatory clinics. Through this program, we hope to implement several educational strategies for providers and patients, evaluate and measure the effectiveness of these strategies, and improve on them to achieve our goal of 50% reduction of inappropriate outpatient antibiotic use by 2020.
References:
- Fleming-Dutra KE et al, JAMA. 2016;315(17):1864., Antimicrob Agents Chemother. 2015;59(7):3848. Epub 2015 Apr 13.
- Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep 2016;65(No. RR-6):1–12
Be Antibiotics Aware Logos Courtesy Centers for Disease Control and Prevention

Dr. Dr. Jasmine Riviere Marcelin is the Associate Medical Director, Nebraska Medicine Antimicrobial Stewardship Program