
The CROI 2026 meeting promises to be a vibrant gathering of thought leaders in HIV treatment, prevention, and cure research. Held from February 22-26, 2026, in Denver, CO, the event will feature groundbreaking research, innovative practices, and insightful discussions. We are also proud to highlight that Kim Scarsi, PharmD, one of our exceptional pharmacist faculty, serves on the CROI Scientific Program Committee, contributing to shaping the scientific agenda for this global meeting. We’re thrilled to amplify the brilliant presenters from our division, each contributing to the advancement of healthcare practices:
UNMC Presentations at CROI 2026
Posters:
- Division Authors: Shawna Sunagawa, Kim Scarsi
Presentation: Delamanid and Linezolid PK in the Treatment of Drug-Resistant Pulmonary TB: Results from ACTG 5356
Time: Poster Session: Wednesday, February 25, 2:30-4pm - Division Authors: Nada Fadul (As part of the National Clinical Cohort Collaborative Team)
Presentation: Prescriptions for Oral vs Injectable HIV Preexposure Prophylaxis – Who is using Injectable PrEP, and How’s That Going?
Time: Poster Session: Tuesday, February 25, 2:30-4pm
Oral Abstracts
Division Authors: Sue Swindells (As part of the A5406 study team author list: Wasserman S, van de Venter R, Harrison L, McKhann A, Ignatius E, Maartens G, Swindells S, Naidoo A, Shenje J, Avihingsanon A, Denti P, Wasmann R, Chaisson RE for the A5406 study team)
Presentation: Twice-Daily Dolutegravir with a 4-Month Rifapentine-Based Regimen for HIV-Associated Tuberculosis
Time: Tuesday February 24- 10:00 AM to 12:00 PM
Meet the Speakers



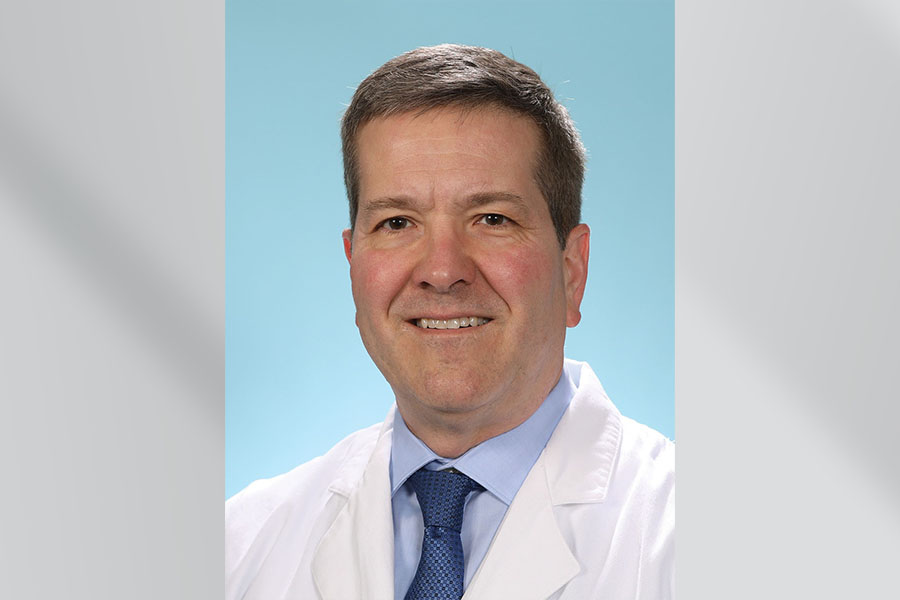
Dr. Shawna Sunagawa is a clinical pharmacist at the Nebraska Medicine Specialty Care Center, where she provides expert medication management for people living with HIV. Her work is integral to supporting ART adherence, managing drug–drug interactions, and helping patients navigate complex treatment plans. She contributes actively to clinical research and multidisciplinary care at UNMC.
Dr. Sue Swindells is a globally recognized HIV researcher whose work has shaped standards of care for HIV treatment and prevention. She has led major NIH- and ACTG‑funded clinical trials, including those focused on long‑acting antiretrovirals and TB/HIV coinfection. Her leadership on the ACTG A5406 study team continues her legacy of bringing evidence-based, innovative therapies to people living with HIV worldwide.
Dr. Kim Scarsi is a distinguished HIV pharmacist and researcher in the UNMC Division of Infectious Diseases. She plays a major role in optimizing HIV therapy, advancing pharmacologic research, and mentoring the next generation of HIV clinicians. Dr. Scarsi has contributed to multiple national and international research collaborations and brings deep expertise in antiretroviral therapy and long‑acting formulations.

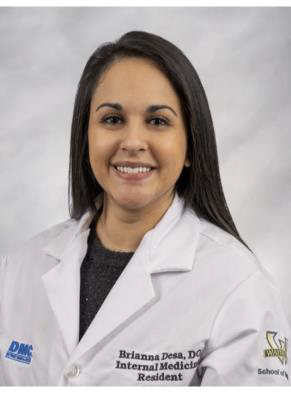
Dr. Nada Fadul is a Professor of Medicine and Associate Dean for Faculty Affairs at the University of Nebraska Medical Center, where she also serves as Principal Investigator for the Ryan White Parts C & D programs. Her work spans HIV clinical care, health equity, and implementation science, with a strong record of publishing in high‑impact journals and presenting at national and international conferences. She is a leader in the HIV Medical Association, serving on its Board of Directors and as Chair of the Awards Committee, and is deeply committed to mentoring trainees and advancing diversity, equity, and inclusion in medical education.
HIV Clinical Care & Research at UNMC
UNMC and Nebraska Medicine have built one of the Midwest’s most comprehensive HIV care and research programs. The UNMC/Nebraska Medicine Specialty Care Center (SCC) has been providing high‑quality HIV clinical care for over 30 years, serving patients from Nebraska, western Iowa, and the broader region.
A Multidisciplinary Model of Excellence
The SCC’s care model includes infectious disease physicians, pharmacists, nurses, behavioral health specialists, case managers, and research staff working together to support every aspect of patient health. Physician leaders such as Dr. Sara Bares (Medical Director of the SCC) and Dr. Nada Fadul (Ryan White Parts C & D Principal Investigator) lead efforts to reduce disparities, expand treatment access, and ensure equitable care across communities.
Leadership in Long‑Acting HIV Treatment
UNMC is also a national leader in long‑acting injectable HIV therapy, which offers an alternative to daily oral medications and helps patients overcome barriers such as pill burden, stigma, and housing or food insecurity. A major grant awarded to Dr. Nada Fadul supports expanding long‑acting therapy beyond Omaha, increasing access for patients across greater Nebraska.
Innovative, Impactful Research including:
- Clinical trials of new antiretroviral therapies and long‑acting formulations
- Studies on HIV/STI prevention, including PrEP, PEP, and doxycycline post-exposure prophylaxis
- Research addressing HIV in women, pregnancy, and LGBTQIA+ populations
- Technology‑supported engagement efforts such as telehealth and text‑based adherence interventions
Join Us at CROI 2026
These exceptional presentations highlight the commitment of our faculty, pharmacists, and researchers to advancing science and improving care for people living with HIV and related infections. Be sure to mark your calendar so you don’t miss these sessions!
If you attend one of our sessions, tag us on Bluesky @unmc-id.bsky.social





Recent Comments