The Department of Health and Human Services HIV guidelines panel currently recommends antiretroviral therapy (ART) consisting of two nucleoside reverse transcriptase inhibitors plus an integrase inhibitor for most treatment naïve HIV infected individuals1. Prior to the advent of integrase inhibitors, the utilization of non-nucleoside reverse transcriptase inhibitor (NNRTI) based regimens had been common. Both efavirenz and rilpivirine had been commonly used although both NNRTI’s present some challenges. Efavirenz related neuropsychiatric adverse effects and drug metabolism enzyme induction properties present challenges for its use. Rilpivirine has been shown to be less efficacious in naïve patients with baseline viral loads greater than 100,000 copies per milliliter or CD4 counts less than 200/cmm. In addition, patients requiring a proton pump inhibitor cannot use rilpivirine due to its need for an acidic environment to be absorbed. An NNRTI without similar restrictions may be beneficial.
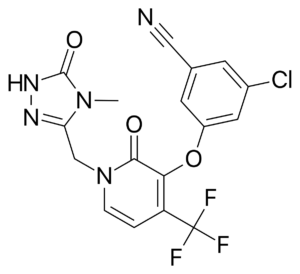 Doravirine (DOR) is a novel NNRTI that provides a similar efficacy for the treatment of HIV infection with activity against HIV variants that are resistant to efavirenz (EFV) and rilpivirine (RPV). Doravirine offers a better safety profile without neuropsychiatric adverse effects, minimal drug-drug interactions and is unaffected by food intake and need for an acidic absorption environment. In August, 2018, doravirine was approved by the FDA for use and will be available solely (Pifeltro™) or as a single tablet regimen (Delstrigo™) in combination with lamivudine (3TC) and tenofovir disoproxil fumurate (TDF).
Doravirine (DOR) is a novel NNRTI that provides a similar efficacy for the treatment of HIV infection with activity against HIV variants that are resistant to efavirenz (EFV) and rilpivirine (RPV). Doravirine offers a better safety profile without neuropsychiatric adverse effects, minimal drug-drug interactions and is unaffected by food intake and need for an acidic absorption environment. In August, 2018, doravirine was approved by the FDA for use and will be available solely (Pifeltro™) or as a single tablet regimen (Delstrigo™) in combination with lamivudine (3TC) and tenofovir disoproxil fumurate (TDF).
Two phase III trials, DRIVE-AHEAD and DRIVE-FORWARD, provided the basis for FDA approval. The summary of these trials follows.
 DRIVE-AHEAD2: A randomized, double-blind, phase III trial compared doravirine to another NNRTI, efavirenz. Adults with HIV-1 infection naïve to ART, HIV RNA >1,000 copies/ml, and CD4 >100/mm3 were randomized to receive DOR 100mg with 3TC 300mg/TDF 300mg or EFV 600mg with TDF 300mg/emtricitabine (FTC) 200mg. The primary endpoint of the study measured virologic response with the proportion of patients achieving HIV RNA <40 copies/ml at week 48. Comparisons between each arm were similar, 77% in DOR arm vs. 78% in EFV arm, demonstrating non-inferiority. Clinical adverse events deemed drug-related were reported in 31% of patients in DOR arm and 56% in EFV arm. Dizziness (6.5% DOR vs. 25% EFV) and abnormal dreams (5.6% DOR vs. 14.8% EFV) had the largest variation between the two groups. Only one emergent NNRTI mutation arose to the DOR group, K101K/E mutation, which causes intermediate resistance to RPV and low-level resistance to EFV.
DRIVE-AHEAD2: A randomized, double-blind, phase III trial compared doravirine to another NNRTI, efavirenz. Adults with HIV-1 infection naïve to ART, HIV RNA >1,000 copies/ml, and CD4 >100/mm3 were randomized to receive DOR 100mg with 3TC 300mg/TDF 300mg or EFV 600mg with TDF 300mg/emtricitabine (FTC) 200mg. The primary endpoint of the study measured virologic response with the proportion of patients achieving HIV RNA <40 copies/ml at week 48. Comparisons between each arm were similar, 77% in DOR arm vs. 78% in EFV arm, demonstrating non-inferiority. Clinical adverse events deemed drug-related were reported in 31% of patients in DOR arm and 56% in EFV arm. Dizziness (6.5% DOR vs. 25% EFV) and abnormal dreams (5.6% DOR vs. 14.8% EFV) had the largest variation between the two groups. Only one emergent NNRTI mutation arose to the DOR group, K101K/E mutation, which causes intermediate resistance to RPV and low-level resistance to EFV.
 DRIVE-FORWARD3: A randomized, controlled, double-blind, phase III, non-inferiority trial compared doravirine to ritonavir-boosted darunavir, a protease inhibitor. Adults with HIV-1 infection naïve to ART, with plasma HIV RNA >1,000 copies/ml were screened and randomized to receive DOR 100mg or DRV 800mg/RTV 100mg (DRV/r), in combination with either TDF/FTC or ABC/3TC based on investigator choice. The proportion of patients that achieved plasma HIV-1 RNA <50 copies/ml at week 48 defined the primary endpoint of this trial. Doravirine showed non-inferiority to ritonavir boosted darunavir, with 84% in DOR arm vs. 80% in DRV/r arm achieving success with HIV RNA <50c/ml at week 48. Clinical adverse events due to drug therapy were reported in 31% in DOR and 32% in DRV/r group, with diarrhea comprising 5% of DOR patients vs. 13% of DRV/r patients. Lab abnormalities were similar between the two regimens, except LDL-cholesterol increases in <1% of DOR patients vs. 9% of DRV/r patients. Resistance testing was performed in 15 protocol-defined virologic failure (PDVF) patients, and within this group no emergent mutations to DOR were found. One case of resistance was found in a patient that discontinued treatment because of non-compliance at week 24, thus was not included in the PDVF category, encompassing resistance to DOR (V106I, H221Y, F227C) and FTC (M184V).
DRIVE-FORWARD3: A randomized, controlled, double-blind, phase III, non-inferiority trial compared doravirine to ritonavir-boosted darunavir, a protease inhibitor. Adults with HIV-1 infection naïve to ART, with plasma HIV RNA >1,000 copies/ml were screened and randomized to receive DOR 100mg or DRV 800mg/RTV 100mg (DRV/r), in combination with either TDF/FTC or ABC/3TC based on investigator choice. The proportion of patients that achieved plasma HIV-1 RNA <50 copies/ml at week 48 defined the primary endpoint of this trial. Doravirine showed non-inferiority to ritonavir boosted darunavir, with 84% in DOR arm vs. 80% in DRV/r arm achieving success with HIV RNA <50c/ml at week 48. Clinical adverse events due to drug therapy were reported in 31% in DOR and 32% in DRV/r group, with diarrhea comprising 5% of DOR patients vs. 13% of DRV/r patients. Lab abnormalities were similar between the two regimens, except LDL-cholesterol increases in <1% of DOR patients vs. 9% of DRV/r patients. Resistance testing was performed in 15 protocol-defined virologic failure (PDVF) patients, and within this group no emergent mutations to DOR were found. One case of resistance was found in a patient that discontinued treatment because of non-compliance at week 24, thus was not included in the PDVF category, encompassing resistance to DOR (V106I, H221Y, F227C) and FTC (M184V).
In summary, doravirine paired with 3TC/TDF demonstrates similar efficacy to regimens anchored by efavirenz or ritonavir boosted darunavir at week 48 in HIV infected treatment naïve patients. Doravirine demonstrated an acceptable tolerability and safety profile with very little treatment emergent ART resistance mutations. Studies investigating a switch to DOR/3TC/TDF in virologically suppressed experienced patients (DRIVE-SHIFT) and in ART naïve patients with NNRTI transmitted resistance are currently ongoing. However, comparisons of doravirine based regimens versus any of the currently recommended INI based regimens is unknown.
References:
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. Department of Health and Human Services. March 2018. Available at: http://aidsinfo.nih.gov/contentFiles/AdultandAdolescentGL.pdf. [Accessed 4 September 2018].
- Orkin C, Squires KE, Molina JM, et al. Doravirine/lamivudine/TDF is noninferior to efavirenz/emtricitabine/TDF in treatment naïve adults with HIV-1 infection: week 48 results of the phase 3 DRIVE-AHEAD study. Clinical Infect Dis. (Submitted).
- Molina JM, Squires K, Sax P, et al. Doravirine versus ritonavir-boosted darunavir in antiretroviral naïve adults with HIV-1 infection (DRIVE-FORWARD): 48-week results from a randomized, double-blinded, phase 3, non-inferiority trial. Lancet HIV 2018; 5e211-e220.

Content provided by Kelsey Christensen, 4th year PharmD Candidate, and Josh Havens PharmD, Specialty Care Clinic Pharmacy Coordinator
