This post is part of a series recognizing Antimicrobial Awareness Week 2024. Today, we are sharing some examples of clinical situations where shorter antibiotic duration of treatment are recommended. This post was written by Jeremy Tigh, PharmD.
The duration of antibiotic therapy for bacterial infections historically reflected long-standing dogma and relied largely on expert opinion and tradition. In the setting of a lack of high-quality data, and early false concerns for the development of resistance with short durations, longer fixed durations of therapy were sought after knowing that overtreatment occurred but ensured that every patient was “maximally cured.”1-2 In 2010 Paul Sax, MD wrote a satirical piece in the New England Journal of Medicine’s blog highlighting the lore in figuring out the length of antibiotic therapy, using non-evidence-based multiples of 5 (fingers on a hand) or 7 (days of the week).3 Since that piece, there has been an ongoing push towards studying proper durations of therapy, a movement dubbed “Shorter is Better” by expert in the field Brad Spellberg, MD.4-7 This refers to shortening the number of days an antibiotic course is given, while not increasing risk for treatment failure. This leads to less risk of harm including decreased antibiotic resistance, fewer adverse effects, and less Clostridioides difficile infection. Newer evidence supports shorter durations for some common infections. It is the goal of this document to encourage translating this evidence into current practice.
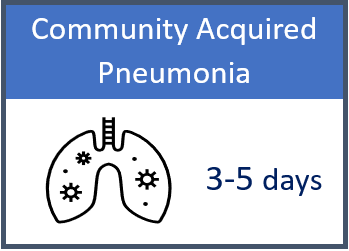
Key Points8-10: Since 2019, IDSA has endorsed 5 days of antibiotics for patients with CAP who are clinically improving on therapy. A recent randomized controlled trial found antibiotics could be safely stopped at 3 days in patients who met markers for clinical stability (afebrile 48-72 hours, spO2 >90%, etc.). In patients with an initially elevated procalcitonin, antimicrobials can be stopped when it returns to normal (<0.25 ng/mL) or decreases by ³80%. Extra-pulmonary infections or those with infections caused by Pseudomonas aeruginosa or Staphylococcus aureus may require longer courses of treatment.
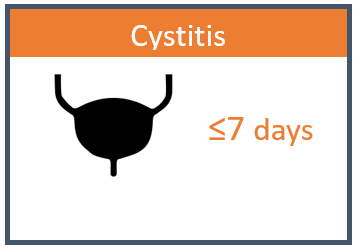
Key Points11-14: For uncomplicated cystitis, evidence supports 3 days of TMP-SMX (Bactrim) or 5 days of nitrofurantoin. Alternate options include 3 days of fluoroquinolones or 5 days of a beta-lactam (e.g., amoxicillin-clavulanate, cephalexin, cefuroxime). For complicated cystitis (including catheterized patients and those with urologic abnormalities), evidence supports 7 days of treatment. For pyelonephritis, longer courses of 7 days (fluoroquinolone) to 10-14 (TMP/SMX, beta-lactams) days are appropriate. Bacteria in the urine without any urinary symptoms is considered asymptomatic bacteriuria and should NOT be treated (exceptions: pregnancy, impending urologic surgery).
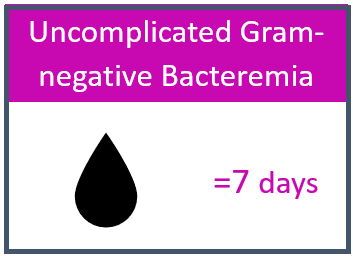
Key Points15-18: Multiple studies have demonstrated that 7 days of total antibiotic therapy is noninferior to 14 days in clinically stable patients who have adequate source control. Conversion to oral antibiotics is appropriate in patients who demonstrate clinical improvement while on IV therapy. Should use an oral antibiotic with demonstrated susceptibility against causative pathogen and high bioavailability (TMP/SMX, levofloxacin, cephalexin, amoxicillin-clavulanate). Longer durations may be necessary for immunocompromised patients, those with inadequate source control, or for certain pathogens such as Pseudomonas aeruginosa.
Key Points19-21: Treatment for 5-7 days is appropriate for most patients if there has been improvement in symptoms. Longer courses may be required for severe infections or infections without source control (undrained abscess). Diabetes alone is not an indication for a longer course
Key Points22-23: More than 1 in 5 antibiotics prescribed in adults are for sinusitis. In adults, acute bacterial rhinosinusitis should only be diagnosed when symptoms persist without evidence of improvement for at least 10 days beyond the onset of symptoms or after double worsening. In adults, 5-7 days of therapy is appropriate if improvement after 3-5 days of treatment occurs: 7-10 days if delayed response or switch to alternative therapy due to lack of response (Augmentin). In children, longer treatment duration of 10-14 days is recommended.
Key Points24: 10 days for penicillin, amoxicillin, 1st generation oral cephalosporins, clindamycin. 5 days for azithromycin (not preferred due to increasing macrolide resistance)

Key Points25: Amoxicillin, amoxicillin-clavulanate (preferred if antibiotic exposure within 30 days, recurrent infection), or oral cephalosporins: For children <2 years and children (any age) with tympanic membrane perforation or history of recurrent infection: 10 days. For children >2 years with intact tympanic membrane and no history of recurrent AOM 5-7 days.
References:
Document adapted from Public Health Ontario: Shorter is Smarter Resources.
- Llewelyn M J, Fitzpatrick J M, Darwin E, Tonkin-Crine S, Gorton C, Paul J et al. The antibiotic course has had its day BMJ 2017; 358 :j3418 doi:10.1136/bmj.j3418
- Rice LB. The Maxwell Finland Lecture: for the duration-rational antibiotic administration in an era of antimicrobial resistance and Clostridium difficile. Clin Infect Dis. 2008;46(4):491-496. doi:10.1086/526535
- https://blogs.jwatch.org/hiv-id-observations/index.php/how-to-figure-out-the-length-of-antibiotic-therapy/2010/10/22/
- Spellberg B, Rice LB. Duration of Antibiotic Therapy: Shorter Is Better. Ann Intern Med. 2019;171(3):210-211. doi:10.7326/M19-1509
- Spellberg B. The Maturing Antibiotic Mantra: “Shorter Is Still Better”. J Hosp Med. 2018;13(5):361.362. doi:10.12788/jhm.2904
- Spellberg, Brad. “The New Antibiotic Mantra-“Shorter Is Better”.” JAMA internal medicine vol. 176,9 (2016): 1254-5. doi:10.1001/jamainternmed.2016.3646
- Spellberg B, Srinivasan A, Chambers HF. New Societal Approaches to Empowering Antibiotic Stewardship. JAMA. 2016;315(12):1229-1230. doi:10.1001/jama.2016.1346
- Metlay JP, Waterer GW, Long AC, et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45-e67. doi:10.1164/rccm.201908-1581ST
- Dinh A, Ropers J, Duran C, et al. Discontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC): a double-blind, randomised, placebo-controlled, non-inferiority trial [published correction appears in Lancet. 2021 Jun 5;397(10290):2150]. Lancet. 2021;397(10280):1195-1203. doi:10.1016/S0140-6736(21)00313-5
- https://www.unmc.edu/intmed/divisions/id/asp/clinical-pathways/docs/CAP-Guidance-2020-Revision-Final-Updated.pdf
- Gupta K, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011;52:e103-20
- Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(5):625-663. doi:10.1086/650482
- Drekonja DM, Trautner B, Amundson C, Kuskowski M, Johnson JR. Effect of 7 vs 14 Days of Antibiotic Therapy on Resolution of Symptoms Among Afebrile Men With Urinary Tract Infection: A Randomized Clinical Trial. JAMA. 2021;326(4):324-331. doi:10.1001/jama.2021.9899
- https://www.unmc.edu/intmed/divisions/id/asp/clinical-pathways/docs/NM-Updated-UTI-Guidance_Final-1.pdf
- Heil EL, Bork JT, Abbo LM, et al. Optimizing the Management of Uncomplicated Gram-Negative Bloodstream Infections: Consensus Guidance Using a Modified Delphi Process. Open Forum Infect Dis. 2021;8(10):ofab434. Published 2021 Oct 11. doi:10.1093/ofid/ofab434
- Yahav D, Franceschini E, Koppel F, et al; Bacteremia Duration Study Group. Seven versus 14 days of antibiotic therapy for uncomplicated gram-negative bacteremia: a noninferiority randomized controlled trial. Clin Infect Dis. 2019;69(7):1091-1098. doi:10.1093/cid/ciy1054
- von Dach E, Albrich WC, Brunel AS, et al. Effect of C-reactive protein–guided antibiotic treatment duration, 7-day treatment, or 14-day treatment on 30-day clinical failure rate in patients with uncomplicated gram-negative bacteremia: a randomized clinical trial. JAMA. 2020;323(21):2160-2169. doi:10.1001/jama.2020.6348
- Molina J, Montero-Mateos E, Praena-Segovia J, et al; SHORTEN trial team. Seven-versus 14-day course of antibiotics for the treatment of bloodstream infections by Enterobacterales: a randomized, controlled trial. Clin Microbiol Infect. Published online September 9, 2021. doi:10.1016/j.cmi.2021.09.001
- Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America [published correction appears in Clin Infect Dis. 2015 May 1;60(9):1448. Dosage error in article text]. Clin Infect Dis. 2014;59(2):e10-e52. doi:10.1093/cid/ciu444
- Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164(15):1669-74
- https://www.unmc.edu/intmed/divisions/id/asp/clinical-pathways/docs/ssti-guidelines-2018.pdf
- Chow AW, et al. IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults. Clin Infect Dis 2012;54:e72-112.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical Practice Guideline (Update): Adult Sinusitis. Otolaryngology–Head and Neck Surgery. 2015;152(2_suppl):S1-S39. doi:10.1177/0194599815572097
- Shulman ST, et al. Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the Infectious Diseases Society of America. Clin Infect Dis 2012;55:e86-102
- Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media [published correction appears in Pediatrics. 2014 Feb;133(2):346. Dosage error in article text]. Pediatrics. 2013;131(3):e964-e999. doi:10.1542/peds.2012-3488