 As our institution, state, country, and the world grapple with the impacts of SARS-CoV-2, causing COVID19, there are lots of ongoing discussions about coronaviruses.
As our institution, state, country, and the world grapple with the impacts of SARS-CoV-2, causing COVID19, there are lots of ongoing discussions about coronaviruses.
Dr. Raquel Lamarche is a PGY1 Internal Medicine/Pediatrics resident at UNMC, who will be summarizing updates about SARS-CoV-2 and hopefully make information easier to digest, with additional outlines of implications for graduate medical education.
TODAY’S PRIMER: Human Coronaviruses (HCoVs)
Four HCoVs cause mild upper respiratory infections (common cold): 229E, OC43, NL63, and HKU1. Less frequently, these can be associated with lower respiratory tract infections, primarily in infants and the immunocompromised.
Three HCoVs are related to lower respiratory infections and responsible for recent epidemics:
 1. SARS-CoV-1. This virus was responsible for the 2002-2003 global outbreak of severe acute respiratory syndrome (SARS). The virus causes a spectrum of disease, including asymptomatic infections and mild illness.
1. SARS-CoV-1. This virus was responsible for the 2002-2003 global outbreak of severe acute respiratory syndrome (SARS). The virus causes a spectrum of disease, including asymptomatic infections and mild illness.
The outbreak lasted for 9-months, resulting in 8096 reported cases and 774 deaths. SARS-CoV disproportionately affected adults, who typically presented with fever, myalgia, headache, malaise, followed by dyspnea 5-7 days later. 25% of adults developed watery diarrhea. 20% developed respiratory distress requiring intubation and mechanical ventilation.
The overall mortality rate was 10%, with most deaths occurring in the 3rd week of illness. The case-fatality rate in people older than 60 approached 50%. Notably, no infant or child deaths were documented. The horseshoe bat is the natural reservoir of SARS-CoV-like viruses. The virus is thought to have evolved through civet cats or intermediate animal hosts in the wet markets of China.
The 2002-2003 global outbreak was controlled due to the rapid identification of cases, contact tracing, quarantine, and isolation. We always wondered whether a large scale re-emergence of SARS-CoV would ever occur and as Italians would say, “eccoci qui,” here we are.
 2. MERS-CoV. This was a novel virus identified in 2012. The disease caused by this virus was called Middle-East respiratory syndrome (MERS).[It is important to note that while this virus and disease were unfortunately named for the region of the world where they were identified, it is generally recommended to avoid naming diseases after geographic regions, race/ethnicity, etc., as this can lead to stigma associated with the disease].
2. MERS-CoV. This was a novel virus identified in 2012. The disease caused by this virus was called Middle-East respiratory syndrome (MERS).[It is important to note that while this virus and disease were unfortunately named for the region of the world where they were identified, it is generally recommended to avoid naming diseases after geographic regions, race/ethnicity, etc., as this can lead to stigma associated with the disease].
MERS is associated with a severe respiratory illness similar to that with SARS-CoV, resulting in 2494 cases and 858 deaths. Cases continue today but are primarily contained in the Middle East. Data suggests that the virus evolved from bats, with dromedary camels acting as intermediate hosts.
Preventing transmission from camels is challenging, given the prevalent use of camels in some Middle Eastern countries. The case-fatality rate is high, estimated at 35%, but may partially reflect surveillance bias for more severe disease. (Red Book, 31st edition)
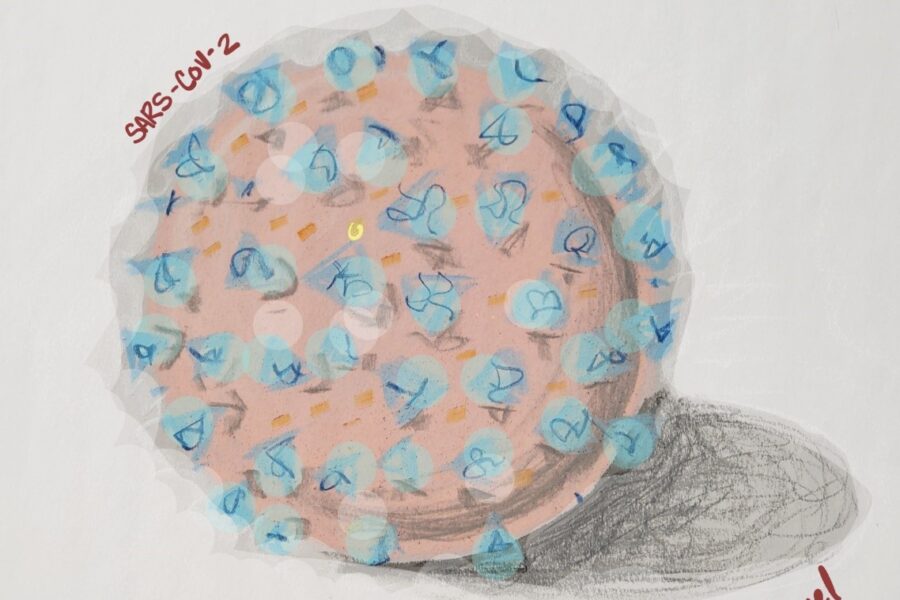
 3. SARS-CoV-2. This is the virus causing the current pandemic. The disease, now known as COVID-19, was first reported in Wuhan, China, in late December 2019. Click the link for the current number of US cases. This virus likely originated in chrysanthemum bats. There is probably an intermediate host between bats and humans, and preliminary data suggest it is the pangolin.
3. SARS-CoV-2. This is the virus causing the current pandemic. The disease, now known as COVID-19, was first reported in Wuhan, China, in late December 2019. Click the link for the current number of US cases. This virus likely originated in chrysanthemum bats. There is probably an intermediate host between bats and humans, and preliminary data suggest it is the pangolin.
The virus uses a densely glycosylated spike (S) protein to enter host cells and binds with high affinity to the angiotensin-converting enzyme 2 (ACE2) receptor in humans like SARS-CoV. It is still unclear why SARS-CoV-2 is more easily transmissible than SARS-CoV-1 or MERS-CoV.
This virus is actively mutating, which means the virulence and transmission will shift over time in unpredictable ways. See genomic epidemiology of novel coronavirus. Genetic analyses of 103 SARS-CoV-2 genomes indicated that we have two different types of the virus:
• L Haplotype (∼70%) is more prevalent and causes more severe illness
• S Haplotype (∼30%), less prevalent, and causes milder illness
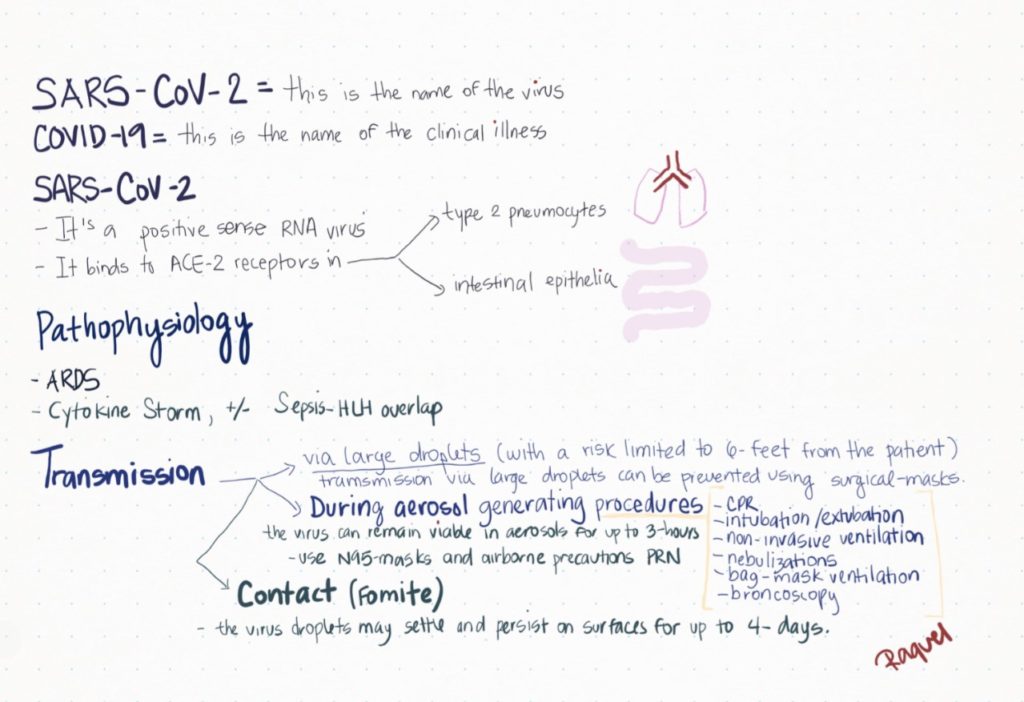
SARS-CoV-2: severe acute respiratory syndrome coronavirus-2; COVID-19: coronavirus disease-2019; ACE-2: angiotensin converting enzyme-2; ARDS: acute respiratory distress syndrome; HLH: hemophagocytic lympho-histiocytosis; PRN: as needed, CPR: cardio-pulmonary resuscitation
Transmission is via LARGE D-R-O-P-L-E-T-S. Droplet transmission is prevented by using standard surgical-masks. If those droplets are aerosolized, the virus can prevail for up to 3 hours in the aerosols. The CDC recommends airborne precautions especially during aerosol-generating procedures (sputum induction, open suctioning of airways, intubation, tracheostomy, CPAP, bag-mask ventilation).
Contact transmission implies virus-containing droplets settling on surfaces, a person touching such contaminated surfaces/objects and transferring the virus to their faces and mucous membranes. The virus can survive for up to four days on surfaces. To prevent this form of transmission, you can:
• Avoid touching your face (I’m sure your face is itching now)
• Disinfecting surfaces with 0.5% sodium hypochlorite
• Cleaning hands with an alcohol-based sanitizer
• Be mindful of your stethoscope and sanitize it often
Clinical Overview: Incubation 2-14 days; median of 4-5 days. Rare patients may have a more prolonged incubation of up to 24 days; this potentially long incubation period could have implications for quarantine policies and prevention of spread. Clinical signs/symptoms include:
• Upper respiratory infection symptoms
• Lower respiratory symptoms (shortness of breath)
• Fever (may not be present in up to 50% of cases)
• Less commonly, gastrointestinal symptoms like diarrhea or nausea in 10% of patients
• The elderly may have hypoxemia with no increased work of breathing
• Physical examination is nonspecific
• Lymphopenia is present in ~80% of patients
• Elevated CRP in 60% of the patients. Poor prognostic factor
• SARS-CoV-2 is not associated with elevated procalcitonin (95% patients had pro-calcitonin below 0.5)
In future Weekly Corona posts, we will explore what we know about personal protective equipment for COVID-19, treatment options, impacts on medical education, and more. Stay tuned!
Endnote: As we sift through the mountains of information about COVID-19, it is helpful to keep a few reliable resources bookmarked. Review these often, at least weekly, for updates:
• World Health Organization https://www.who.int/emergencies/diseases/novel-coronavirus-2019
• Centers for Disease Control & Prevention https://www.cdc.gov/coronavirus/2019-ncov/index.html
• Infectious Diseases Society of America https://www.idsociety.org/public-health/COVID-19-Resource-Center/
• Nebraska Medicine https://www.nebraskamed.com/for-providers/covid19
• University of Washington https://covid-19.uwmedicine.org/Pages/default.aspx
• Our World in Data https://ourworldindata.org/coronavirus
Gracias Dra Lamarche, útil y claro, un gran recurso para mantenerse actualizado en lo importante, un fuerte abrazo desde INTEC, contento de saber de ti.
Aprecio mucho su comentario. Deseando que usted y su familia se encentren sanos.