The following was originally posted to the Controversies in Hospital Infection Prevention Blog on 9/24/18 by Dr. Marcelin.
September 28, 2018 marks 90 years since Sir Alexander Fleming discovered penicillin as an effective antimicrobial which would soon save millions of lives. He warned soon afterwards that unless we used penicillin judiciously, we would see antibiotic resistance, and he was right. With decades of inappropriate antibiotic prescribing, we have dug ourselves a deep hole of antimicrobial resistance, and inaccurate penicillin allergies is but one shovel used to put us in this mess. How? Simple If/And/Then construct: IF unverified penicillin allergies lead to unnecessary/inappropriate use of broad-spectrum antibiotics which contributes to antimicrobial resistance, AND antimicrobial resistance is a public health problem, THEN unverified penicillin allergies are a public health problem.
In a single day on hospital service the Infectious Diseases consult team encountered a few patients with beta lactam allergies: one had developed significant angioedema in the last year with amoxicillin; another had developed a questionable rash on nafcillin therapy; a third recalled his mother telling him that he turned green after receiving oral penicillin as a child. Our approach: in the first case we avoided penicillin; in the second, we recommended a cephalosporin graded challenge which the patient tolerated; in the third, after detailed history we gave the patient full dose amoxicillin-clavulanate, he tolerated it well and he was able to discharge without IV antibiotics. These are fantastic cases for teaching purposes, but additionally, how exhilarating it is to liberate a patient from an irrelevant penicillin “allergy” and give them appropriate treatment upfront!
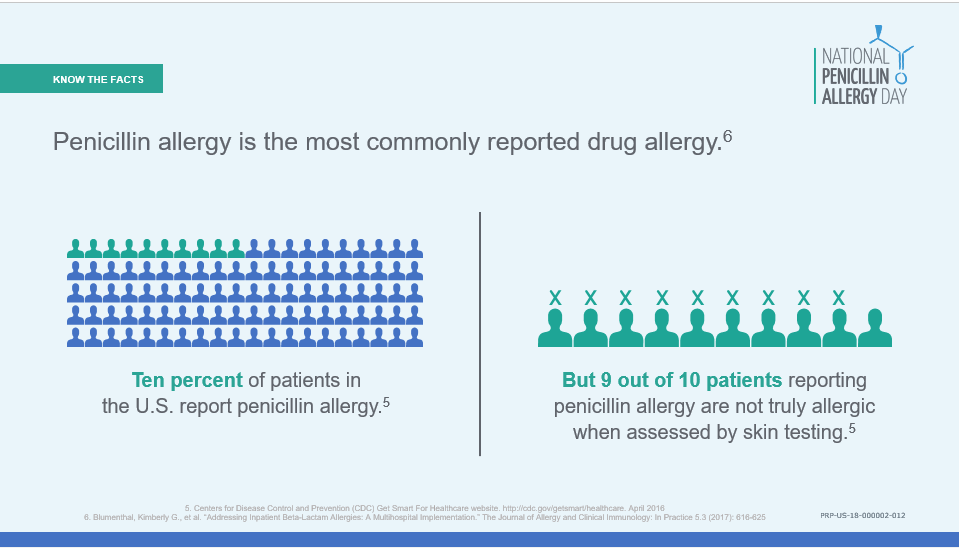 Penicillin allergies are frequently documented drug allergies in the hospital setting, with 10% of Americans reporting a penicillin allergy. Some penicillin allergies are real. However, most penicillin allergies are either inaccurate or inconsequential, with only 1% of Americans actually demonstrating true allergy upon testing. Furthermore, most patients with true penicillin allergies lose hypersensitivity over time, and by 10 years after the event, 80% of patients are no longer penicillin allergic. Can you imagine if all potential food allergies were treated the same as penicillin allergies? People wouldn’t eat at all! Most people, if they have what they think might be a reaction to a food they like, might either try the food again or get tested to know for certain they cannot eat that food. But 50 years ago, if they had a rash that coincided with penicillin administration, it would never occur to them to try it again.
Penicillin allergies are frequently documented drug allergies in the hospital setting, with 10% of Americans reporting a penicillin allergy. Some penicillin allergies are real. However, most penicillin allergies are either inaccurate or inconsequential, with only 1% of Americans actually demonstrating true allergy upon testing. Furthermore, most patients with true penicillin allergies lose hypersensitivity over time, and by 10 years after the event, 80% of patients are no longer penicillin allergic. Can you imagine if all potential food allergies were treated the same as penicillin allergies? People wouldn’t eat at all! Most people, if they have what they think might be a reaction to a food they like, might either try the food again or get tested to know for certain they cannot eat that food. But 50 years ago, if they had a rash that coincided with penicillin administration, it would never occur to them to try it again.
 Once a penicillin allergy is listed in a patient’s record, they are more likely to receive inappropriate broad-spectrum antibiotics – a practice that can be both costly and have worse clinical outcomes. Patients with methicillin-susceptible Staphylococcus aureus bacteremia treated with vancomycin instead of a beta-lactam have higher mortality rates than those receiving appropriate beta-lactam therapy. Patients undergoing surgery who receive alternative antibiotics for preoperative infection prophylaxis (due to reported penicillin allergies) have a 50% higher risk of developing a surgical site infection than those who appropriately receive beta lactam prophylaxis.
Once a penicillin allergy is listed in a patient’s record, they are more likely to receive inappropriate broad-spectrum antibiotics – a practice that can be both costly and have worse clinical outcomes. Patients with methicillin-susceptible Staphylococcus aureus bacteremia treated with vancomycin instead of a beta-lactam have higher mortality rates than those receiving appropriate beta-lactam therapy. Patients undergoing surgery who receive alternative antibiotics for preoperative infection prophylaxis (due to reported penicillin allergies) have a 50% higher risk of developing a surgical site infection than those who appropriately receive beta lactam prophylaxis.
The Infectious Disease Society of America (IDSA) and Society of Healthcare Epidemiology of America (SHEA) recommend that patients with reported beta lactam allergy should undergo beta lactam allergy skin testing. Allergy verification and penicillin allergy skin-testing are becoming more recognized components of antimicrobial stewardship and de-labelling allergies can have significantly improved patient outcomes. Following a simple algorithm can help to easily identify patients suitable for skin testing and could avoid almost 3 weeks hospitalization and 1000 days of second-line antibiotics. However in some situations or in low-resource settings, it may not be practical to perform skin testing on everyone who reports a penicillin allergy. In a previous blog post about beta-lactam skin testing I mused about whether better allergy histories are more bang for the buck, since a structured allergy history can potentially decrease inappropriate 2nd line antibiotic use by 26%.
 There’s an age-old joke that if a team wants a detailed history on a patient, just consult ID. If our attention to detail is already expected, shouldn’t we feel empowered to take that allergy history and de-label the penicillin allergy? Inpatient allergy consultations are difficult to coordinate when those divisions may be understaffed and allergists are busy with outpatient practices. So how can we capitalize on their expertise when they can’t see the patient in the hospital? Simple: partner with them to create guidance for practice, utilize ordersets for allergy de-labelling and facilitate outpatient allergy evaluations after discharge.
There’s an age-old joke that if a team wants a detailed history on a patient, just consult ID. If our attention to detail is already expected, shouldn’t we feel empowered to take that allergy history and de-label the penicillin allergy? Inpatient allergy consultations are difficult to coordinate when those divisions may be understaffed and allergists are busy with outpatient practices. So how can we capitalize on their expertise when they can’t see the patient in the hospital? Simple: partner with them to create guidance for practice, utilize ordersets for allergy de-labelling and facilitate outpatient allergy evaluations after discharge.
 In honor of Sir Alexander Fleming and National Penicillin Allergy Day, let us pledge to emancipate our patients from the fake allergies. Go on, get that detailed history! Get some penicillin skin testing! Do that graded challenge! Give that first line beta-lactam antibiotic! But for goodness’ sake when you do, please DELETE the allergy from the health record so that the ordeal does not have to be repeated!
In honor of Sir Alexander Fleming and National Penicillin Allergy Day, let us pledge to emancipate our patients from the fake allergies. Go on, get that detailed history! Get some penicillin skin testing! Do that graded challenge! Give that first line beta-lactam antibiotic! But for goodness’ sake when you do, please DELETE the allergy from the health record so that the ordeal does not have to be repeated!