Tag: history
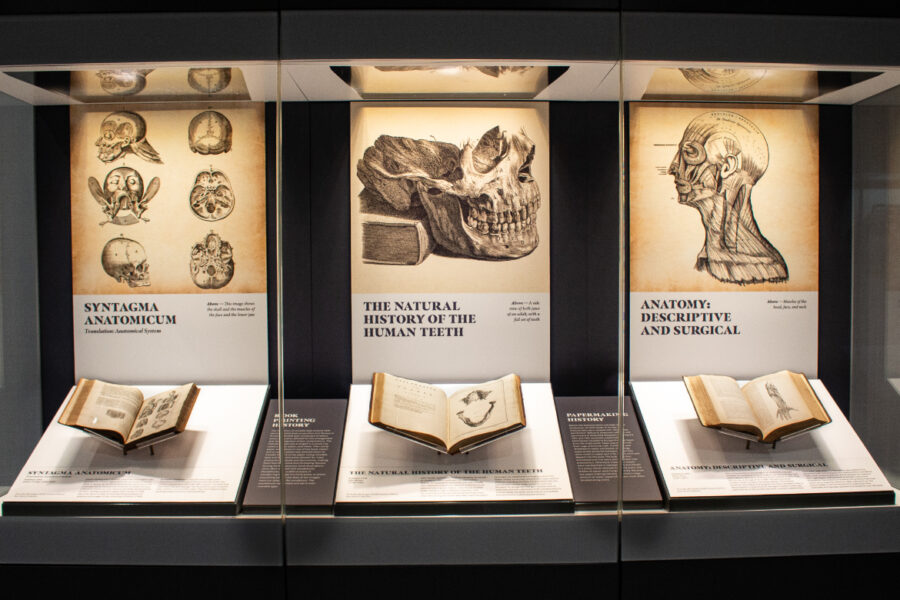
Step Back into Health Sciences History through Rare Books
Recently, the Wigton Heritage Center Rare Book Gallery on Level 5 in Wittson Hall rotated with eight new books. The exhibition features four books from the H. Winnett Orr Rare Book Collection and four books from the library’s Rare Book collection. Erin Torell, rare books librarian at McGoogan Library, shares what visitors can expect to […]
Jun 4, 2025
Now on Display: Jeffrey P. Gold, MD, Collection
Discover the latest donations to the McGoogan Health Sciences Library’s Robert S. Wigton Department of Special Collections and Archives. This latest rotation features items from the Jeffrey P. Gold, MD, Collection highlighting his time as chancellor of UNMC and his support of biopreparedness initiatives. Head to Level 4 of Wittson Hall near the Sorrell Center […]
May 12, 2025

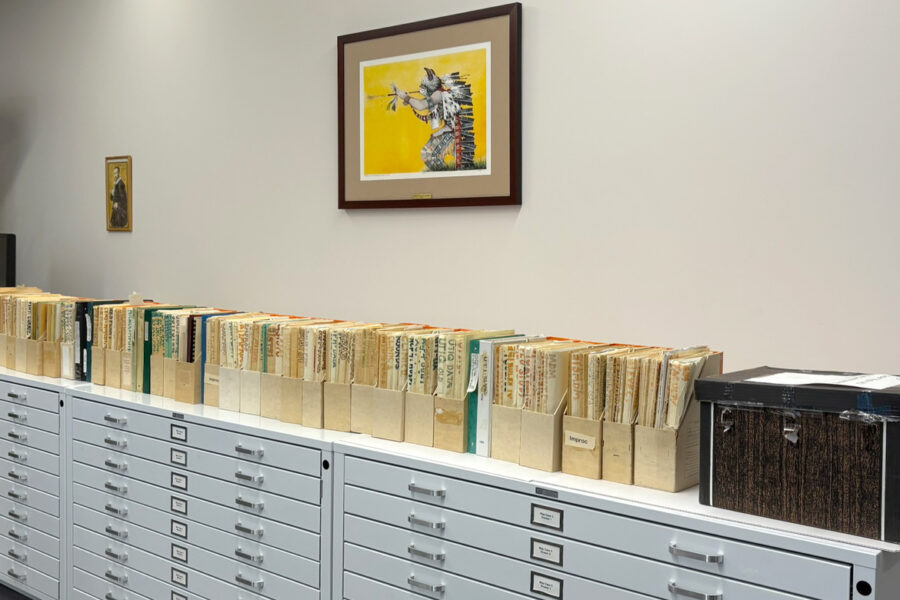
Unpacking and Processing a Legacy: The Robert S. Wigton Collection
Author Kelly Gonzalez, Archives Specialist Archives staff and our volunteer recently finished a several months long project evaluating and preparing the Robert S. Wigton collection for processing. The collection originally consisted of over 85 linear feet of archival material, legacy media, and slides documenting Dr. Wigton’s extensive career as a physician, professor, and campus leader for […]
May 6, 2025
For Now and the Future: McGoogan Library’s Oral History Program
Blog author Grace Spaulding, Student Worker Many UNMC students, faculty, staff and alumni, along with Nebraska Medicine colleagues, have filed into the Level 8 south rare book room of the library to share their stories for the oral history program. With the intention of preserving their lived experience for researchers now and in the future, this […]
May 2, 2025

Davis Lecture Recording Available
Couldn’t attend the Davis Lecture? A recording of author Maria Smilios’ presentation is available online. Maria’s presentation “Sickness & Stigma at Sea View: The Black Angels” covered the deadly disease of tuberculosis and the untold story of the nurses (the Black Angels) who cared for those patients. “The Black Angels” is the true story of […]
Apr 30, 2025